AMERICAN HEART ASSOCIATION (AHA)
Women with a history of diabetes during pregnancy (gestational diabetes) are twice as likely to develop calcium in the heart arteries in middle age, a strong predictor of heart disease, even if healthy blood sugar levels were achieved many years after pregnancy, according to new research published today in the American Heart Association’s flagship journal Circulation .
Gestational diabetes affects approximately 9% of pregnancies in the US and up to 20% worldwide. After pregnancy, women who had gestational diabetes have a higher risk of developing prediabetes or type 2 diabetes, conditions that are risk factors for cardiovascular disease.
Previous studies found a much higher risk of heart disease in women with a history of gestational diabetes who later developed type 2 diabetes. However, it was not clear whether the risk of heart disease among women with a history of gestational diabetes was lower for women who reached healthy glucose levels or who developed prediabetes in middle age.
In 2018, the American College of Cardiology/American Heart Association cholesterol clinical practice guidelines specified that a history of gestational diabetes increases women’s risk of developing arteries that lead to cardiovascular disease.
Using data from the 30-year prospective multicenter Coronary Artery Risk Development in Young Adults (CARDIA) study, researchers investigated whether achieving healthy blood sugar levels after pregnancy would mitigate the increased risk of cardiovascular disease that is associated with a history of of gestational diabetes.
"CARDIA is the first study to evaluate the risk of heart disease in women with a history of gestational diabetes compared to those without gestational diabetes based on their blood sugar levels many years later.
Women with prior gestational diabetes had a two-fold increased risk of coronary artery calcium if they maintained normal blood sugar levels, later developed prediabetes, or were later diagnosed with type 2 diabetes many years after pregnancy compared to women without prior gestational diabetes who had normal blood sugar levels," said Erica P. Gunderson, Ph.D., MS, MPH, epidemiologist and senior research scientist in the Cardiovascular and Metabolic Conditions Section of the Division of Research at Kaiser Permanente. in Oakland, California.
The CARDIA study enrolled more than 5,100 American men and women who were between 18 and 30 years old at the start of the study in 1985. The new analysis includes about 1,100 women (49% black women and 51% white women) without type 1 or type 1 diabetes. 2 who subsequently gave birth at least once during the 25-year study period, which ended in 2011.
Blood tests were performed before and after pregnancy at five-year intervals to determine whether the women had normal blood sugar levels, intermediate elevations in blood sugar levels (prediabetes), or had developed overt Type 2 diabetes.
Heart scans were performed to measure coronary artery calcium , a strong predictor of heart disease, at exams 15, 20, and 25 years after baseline, the first exam in the study.
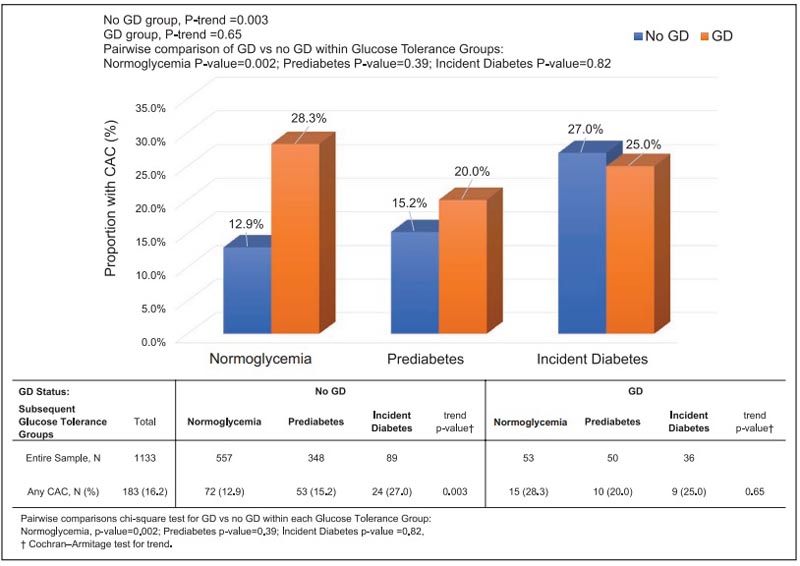 Number (%) of women with any CAC at the end of follow-up (years 15, 20, or 25) by GA status and subsequent glucose tolerance groups. CAC indicates coronary artery calcification; and GD, gestational diabetes.
Number (%) of women with any CAC at the end of follow-up (years 15, 20, or 25) by GA status and subsequent glucose tolerance groups. CAC indicates coronary artery calcification; and GD, gestational diabetes.
At the 25-year follow-up , the average age of participants was 48 years and 12% of the women in the study had a pregnancy complicated by gestational diabetes. The prospective analysis found:
|
"We were surprised to find that women with a history of gestational diabetes have a significantly increased risk of cardiac artery calcification, even if they maintain normal blood sugar levels after pregnancy," Gunderson said.
"Our findings represent a change in this paradigm by showing that normal blood glucose after gestational diabetes is still associated with an increased risk of coronary artery calcium," the authors note.
"Heart disease risk assessment should not wait until a woman has developed prediabetes or type 2 diabetes," Gunderson said. "Diabetes and other health problems that develop during pregnancy serve as precursors to future risk of chronic diseases, particularly heart disease.
Health care systems should integrate a person’s gestational diabetes history into medical records and monitor heart disease risk factors and recommend testing for type 2 diabetes in these women at regular intervals, which is critical to guiding treatment. prevention efforts.
Limitations of the study include that the researchers did not measure coronary artery calcium levels before pregnancy, and that coronary artery calcium scores were used as a surrogate marker for the risk of heart disease, not cardiovascular events.
Clinical perspective What’s new? • Among black and white women with no history of gestational diabetes, progression to glucose intolerance or overt diabetes within 15 years of pregnancy was associated with a gradual increase in relative risk (1.5 to 2.2 times ) of coronary artery calcification in midlife compared with women who maintained normoglycemia. • Among black and white women with a history of gestational diabetes, the relative risk of coronary artery calcification in midlife was 2 times higher for those with normoglycemia, glucose intolerance (prediabetes), or overt diabetes within 15 years. post-pregnancy compared to women without a history of gestational diabetes who maintained normoglycemia. What are the clinical implications? • Sustained normoglycemia among women with prior gestational diabetes may not decrease the future risk of atherosclerotic cardiovascular disease in women during midlife. • A history of gestational diabetes may implicate underlying vascular changes and adversely affect the development of cardiovascular diseases through pathways such as insulin resistance and altered insulin secretion that promote atherogenic plaques independent of dysglycemia. • These findings add to growing evidence that better screening for cardiovascular disease risk factors in women with a history of gestational diabetes is needed to better stratify women’s risk for early prevention of atherosclerotic cardiovascular diseases. |
Discussion
In summary, the development of coronary calcified plaque as measured by CAC is present in some women in middle age. In our study, the relative risk of such coronary plaque was approximately 2 times higher in women with prior gestational diabetes (GD) for all subsequent levels of glucose tolerance, including normoglycemia, than in women without GD and normoglycemia.
Therefore, a history of GD may represent a constellation of risk factors (eg, dyslipidemia, cumulative increases in BP, increased insulin resistance, endothelial dysfunction, or inflammatory responses) that promote atherosclerotic plaque development. in the absence of hyperglycemia.
Insulin resistance and possibly increased inflammation (hs-CRP) among women with prior GD who remained normoglycemic at follow-up in our study is consistent with this hypothesis. GD may be a particularly vulnerable condition of dysmetabolism leading to the initiation and spread of coronary atherogenesis from early lesions to advanced calcified coronary plaque in younger women.
The increased risk of ASCVD among women with a history of GD has been attributed primarily to their younger age at onset of type 2 diabetes and a several-fold increased risk of progression to type 2 diabetes. It is well known that the onset of type 2 diabetes Age 2 to <40 years increases (3.6 to 6.2 times) mortality and cardiovascular outcomes in women.
Our findings represent a change in this paradigm by showing that normoglycemia after a pregnancy with GD was still associated with an increased risk of CAC.
The risk did not increase further with the transition to prediabetes and type 2 diabetes. In contrast, women without previous GD who subsequently developed prediabetes or overt diabetes had a 1.5 and 2.1 times higher risk of CAC, respectively, than those with normoglycemia.
The clinical implications of our findings are that women with prior GD may benefit from improved traditional testing for CVD risk factors (i.e., blood pressure, dyslipidemia, hyperinsulinemia) and perhaps incorporation of GD into risk calculators to improve CVD risk stratification and prevention. Better characterization of GD phenotypes is also needed to assess CVD risk, because GD diagnostic criteria differ between the United States and other countries.
In the CARDIA study, 25.9% of women with GD progressed to diabetes on average 15 years later, which is similar to the cumulative incidence of 16% to 29% after 10 to 20 years of follow-up in contemporary meta-analyses. and in the US population. Life course epidemiological studies are difficult to undertake in population-based clinical settings due to the prolonged time between pregnancy complications and the occurrence of CVD events.
A major limitation of this research, in general, is the lack of routine biochemical testing for diabetes or CVD risk factors among women of childbearing age. The importance of modifiable lifestyle behaviors with the greatest relevance in reducing both diabetes and CVD risk during the first postpartum year (i.e., breastfeeding and sleep) deserve further attention. Additionally, more accurate clinical prediction tools are needed for women that take into account a history of gestational diabetes and other pregnancy complications.
Finally, this study adds to the growing evidence that better screening for CVD risk factors among women with a history of GD is needed to better stratify women’s risk for early prevention of ASCVD.
















