With myopia expected to affect 50% of the world’s population by 2050, the condition is rapidly becoming a global public health problem.
Myopia, which causes distant objects to become blurry, is already reaching epidemic proportions in certain parts of East and Southeast Asia.
For example, in urban areas of Southeast Asia, 80 to 90 percent of children are myopic by the time they complete their secondary education, an increase of more than 20 percent in the last decade. Although often considered simply a minor inconvenience, higher degrees of myopia are associated with sight-threatening eye problems such as glaucoma, myopic retinal degeneration, and retinal detachment later in life.
Interventions to stop myopia
At birth, newborns are typically farsighted , which then slowly declines to the point that between five and seven years of age, children typically have normal vision or a low degree of farsightedness. Myopia is rare in children under six years of age, even in East Asia; However, in high-risk populations, the number of myopes increases dramatically after this age, possibly related to the intensity of the educational system. Although conventional glasses or contact lenses can correct myopia, they do not slow its progression. In recent years, there has been considerable interest in developing and testing interventions to reduce the rate of myopia progression. Since myopia tends to stabilize in late adolescence, interventions to slow the progression of myopia should occur in childhood.
These interventions generally use one of three approaches:
- Optical treatments that use multifocal glasses or special contact lenses.
- Specially designed rigid contact lenses (orthokeratology) usually worn at night to reshape the cornea at the front of the eye to correct myopia and slow progression.
- Pharmacological interventions involving the use of eye drops such as atropine , which act on the focusing system of the eyes and cause biochemical changes that reduce the rate of eye growth.
The latest evidence
A 2023 Cochrane review on interventions for myopia control in children included 64 studies with 11,617 children and compared various optical and pharmacological interventions to slow myopia progression. The review provided moderate-certainty evidence that higher doses of atropine were probably an effective treatment for the control of myopia, with less certain effects for low-dose atropine. However, some children experienced side effects related to the drops, such as difficulty focusing, sensitivity to light, and eye discomfort. In one of the largest studies, about 15% of children stopped therapy due to side effects.
Based on short-term studies, orthokeratology is the most effective optical treatment to delay eyeball elongation. These lenses were often difficult to tolerate, and more than half of children did not complete treatment in some studies. Other types of contact lenses, known as soft multifocal contact lenses , may also reduce the progression of myopia, but there is still some uncertainty about their beneficial effects. Additionally, 60% of the studies included in the review were conducted in East Asia and it is unclear whether the reported effectiveness would extend to other ethnic groups.
Where does this leave us?
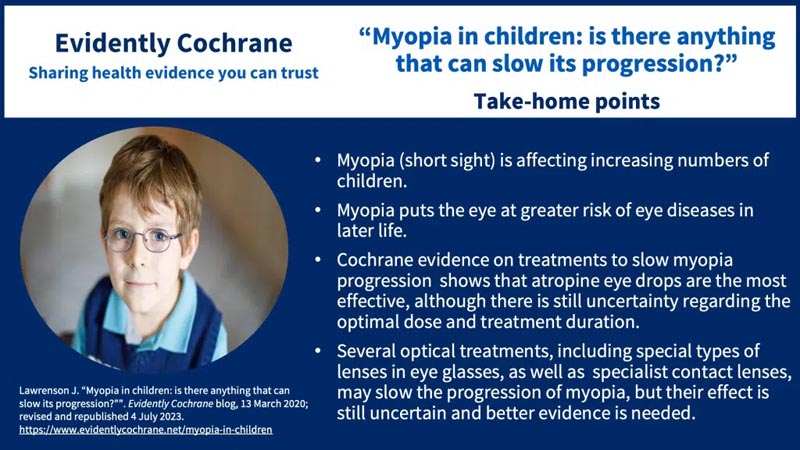
Currently, atropine eye drops appear to be the most effective treatment for myopia control, but more research is needed to determine the optimal dose and duration of therapy. Although lower doses of atropine may reduce side effects, this may be associated with decreased efficacy, but could potentially be used in combination with optical treatments. Optical treatments, including special types of lenses in eyeglasses and contact lenses, can also slow the progression of myopia, but their effect is still uncertain.
Advice for parents of children at risk of developing myopia
An increasing number of eye care professionals offer a variety of pharmacological and optical interventions to slow the rate of myopia progression. Therefore, it is important that parents receive the most up-to-date and relevant evidence about the likely success of these treatments. Therefore, this updated Cochrane review is very timely.
The most effective intervention in the reported studies was atropine eye drops ; however, the concentration of atropine used (0.5%, 1%) was higher than the lowest dose (0.01%) currently offered by most physicians.
As far as optical treatments go, orthokeratology (ortho-K) currently appears to be the most effective treatment for slowing the progression of childhood myopia, but these lenses require more specialized knowledge on the part of the eye care professional and can be difficult to apply. tolerate.
Evidence for the effectiveness of other treatments was limited by the short duration of the studies and considerable variability in treatment response.
Cochrane Review
Interventions for myopia control in children: ongoing systematic review and network meta-analysis
Key messages • Medications such as atropine, administered in the form of eye drops, could slow the progression of myopia in children, and also reduce the elongation of the eyeball due to myopia. The highest doses of atropine are the most effective. The effects of lower doses of atropine are unclear. • Various treatments, including special types of lenses in glasses as well as contact lenses, could slow the progression of myopia, but their effect is still unclear and there is not enough information about the risk of unwanted effects. • It is also unclear whether the reported beneficial effects of medications or lenses on myopia progression are maintained over years. |
Background
Myopia is a common refractive error, in which the elongation of the eyeball causes distant objects to appear blurry. The increasing prevalence of myopia is a growing global public health problem, in terms of rates of uncorrected refractive errors and a significantly increased risk of visual impairment due to myopia-related ocular morbidity. Since myopia is usually detected in children before the age of 10 and can progress rapidly, interventions to slow its progression should be carried out in childhood.
Goals
To evaluate the comparative effectiveness of optical, pharmacological and environmental interventions in slowing the progression of myopia in children using a network meta-analysis (MAR). To generate a relative ranking of myopia control interventions based on their effectiveness. Prepare a brief economic commentary summarizing economic evaluations of myopia control interventions in children. Maintain the currency of evidence through a continuous systematic review approach.
Search methods
We searched CENTRAL (which contains the Cochrane Eyes and Vision Group Trials Register), MEDLINE; Base; and in three test records. The search date was February 26, 2022.
Selection criteria
We included randomized controlled trials (RCTs) of optical, pharmacological and environmental interventions to delay myopia progression in children up to 18 years of age. The key outcomes were myopia progression (defined as the difference in change in spherical equivalent of refraction [SER, diopters (D)] and axial length [mm] in the intervention and control groups at one year or more). and the difference in change in EER and axial length after cessation of treatment ("rebound").
Data collection and analysis
Standard Cochrane methods were used. Bias was assessed using the RoB 2 tool for parallel RCTs. The certainty of the evidence was graded using the GRADE method for the outcomes: change in EER and axial length at one and two years. Most comparisons were made with inactive controls.
Authors’ conclusions
Most studies compared pharmacological and optical treatments to slow myopia progression with an inactive comparator. One-year effects demonstrated that these interventions could slow refractive change and reduce axial elongation, although results were often mixed.
The body of evidence available at two to three years was scarcer, and uncertainty remains about the sustained effect of these interventions. Longer-term, better-quality studies comparing myopia control interventions used alone or in combination, as well as improved methods of monitoring and reporting adverse effects, are needed.
















