In a recent study published in PLoS ONE , researchers examine a wide range of lifestyle variables in the context of multimorbidity from chronic non-communicable diseases.
Summary
Lifestyle factors related to prevalent multimorbidity of chronic diseases: a population-based cross-sectional study
Background
Multimorbidity is associated with poor quality of life, polypharmacy, healthcare costs and mortality, and those affected potentially benefit from a healthy lifestyle. We assessed a comprehensive set of lifestyle factors in relation to multimorbidity with major chronic diseases.
Methods
This cross-sectional study used adult baseline data from the prospective Lifelines cohort in the north of the Netherlands (N = 79,345). We defined multimorbidity as the coexistence of two or more chronic diseases (i.e., cardiovascular disease, cancer, respiratory disease, type 2 diabetes) and evaluated factors in six lifestyle domains (nutrition, physical (in)activity, substance abuse, substances, sleep, stress, relationships) between groups by the number of chronic diseases (≥2, 1, 0).
Multinomial logistic regression models were created, adjusted for appropriate confounders, and odds ratios (ORs) with 95% confidence intervals (95% CI) were reported.
Results
3,712 participants had multimorbidity (4.7%, age 53.5 ± 12.5 years), and this group tended to have less healthy lifestyles .
Compared with those without chronic diseases, those with multimorbidity more frequently reported physical inactivity (OR, 1.15; 95% CI, 1.06–1.25; not significant for a condition), chronic stress (OR , 2.14; 95% CI, 1.92–2.38) and inadequate sleep (OR, 1.70; 95% CI, 1.41–2.06); As expected, they watched television more frequently (OR, 1.70; 95% CI, 1.42–2.04) and currently smoked (OR, 1.91; 95% CI, 1.73–2.11). ), but also consumed less alcohol (OR, 0.66; 95% CI, 0.59–0.74).
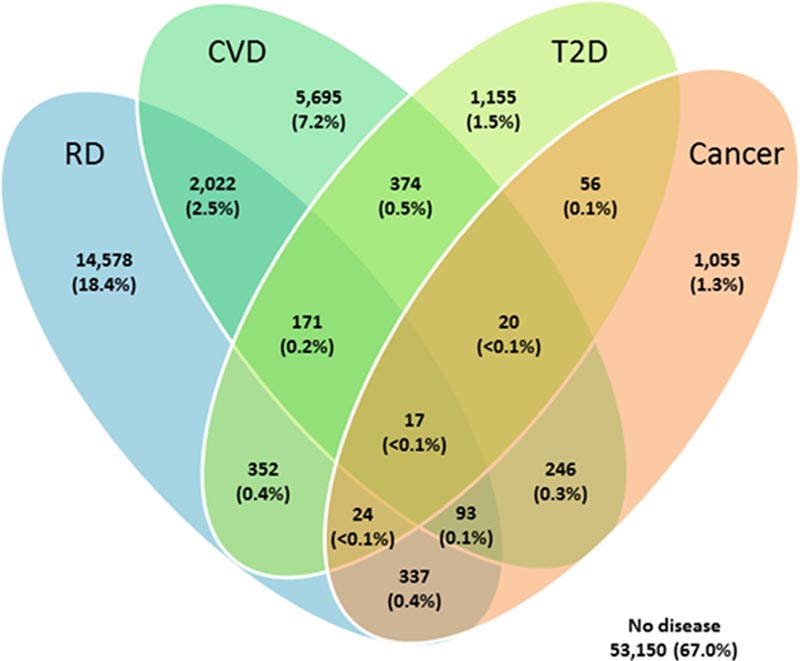
Figure: Overlap in the prevalence of the big four chronic diseases . The big four chronic diseases are respiratory diseases, cardiovascular diseases, type 2 diabetes and cancer. Data are presented as number (%) of a total of 26,195 participants with at least one chronic disease. The complete sample consisted of 79,345 participants, of whom 53,150 did not suffer from any major chronic disease. Abbreviations: CVD, cardiovascular disease; RD, Respiratory disease; T2D, type 2 diabetes.
Conclusions
There is substantial potential to improve physical inactivity and smoking cessation and to work on stress management and sleep hygiene interventions when treating patients with multimorbidity. Studies should now determine the relevance of each lifestyle factor on prognosis, should seek to develop lifestyle interventions for patients living with multimorbidity, and should investigate the impact of these interventions on quality of life and clinical outcomes.
Chronic stress and lack of sleep, in addition to physical inactivity and smoking, are lifestyle factors of great concern in patients with multimorbidity.
Discussion
The most notable findings of this study concern the associations of increased stress and poor sleep with multimorbidity related to the big four chronic diseases. Furthermore, patients with multimorbidity also tended to be physically inactive, in contrast to cases who had a single disease or no major chronic disease.
Although smoking history was associated with the presence of multimorbidity and single disease, the associations were stronger for multimorbidity. Of note, alcohol consumption was lower in subjects with multimorbidity and diet quality was not associated with multimorbidity.
Comments
What is multimorbidity?
Multimorbidity is a global health problem that involves the coexistence of multiple chronic conditions in the same person. Importantly, multimorbidity is linked to cardiovascular disease, respiratory disease, type 2 diabetes, and cancer, leading to higher healthcare costs and higher mortality.
Lifestyle medicine aims to improve clinical care by reducing symptoms, increasing the effectiveness of medications, and promoting disease remission. Understanding the prevalence and specificity of lifestyle multimorbidity risk factors linked to chronic diseases would help determine future clinical treatment recommendations.
About the study
In the present population-based study, investigators evaluate the association between exercise, nutrition, substance abuse, stress, relationships, and sleep with multimorbidity. For the purposes of the present study, multimorbidity was defined as the presence of two or more chronic respiratory diseases, including airflow obstruction and asthma, as well as cardiovascular diseases, type 2 diabetes mellitus (T2D), and cancer.
The study used data from the Lifelines Cohort Study of 79,345 adults living in the northern parts of the Netherlands. Odds ratios (ORs) were calculated using a multivariable logistic regression model, which adjusted for factors such as age, sex, body mass index (BMI), socioeconomic position, educational level, and household income. .
Baseline data were obtained between December 2006 and December 2013 if they contained all lifestyle variables and multimodal outcomes necessary to determine multimorbidity.
Pre-bronchodilator spirometry was used to measure airflow restriction. Asthma was considered present if it was diagnosed by a physician or if the patient was taking asthma medications and had two or more symptoms of wheezing and dyspnea at rest and upon awakening.
Prevalent cases of type 2 diabetes (T2DM) were defined as those who self-documented T2DM or diabetes without type data and those who used diabetes medications or had fasting blood glucose (GFR) of at least 7.0 mmol/L. or glycated hemoglobin (HbA1c) less than 6.5%.
The Lifelines Diet Score (LLDS) was used to assess diet quality, while the Food Frequency Questionnaire (FFQ) was used to analyze diet during the previous month. According to the Short Questionnaire to Assess Health-Enhancing Physical Activity (SQUASH), the Lifelines Physical Activity Score (LLPAS) assessed physical activity.
Acute stress was assessed using the List of Threatening Experiences (LTE), Dutch version, while chronic stress was assessed using the Long-Term Difficulties Inventory (LDI). Self-reported total sleep per 24 hours was classified using the American National Sleep Foundation’s age-specific parameters.
Study findings
About 28% of research participants had a single chronic condition, 5% with multimorbidity and 4.3% with two chronic diseases. Compared with the single-disease and no-disease groups, the multimorbidity group was older and more likely to be overweight or obese. Inadequate sleep was common, with 22% of people with multimorbidity reporting insufficient or slightly inappropriate periods of sleep.
The most common ailment was chronic respiratory disease at 22%, followed by CVD, T2D and cancer at 11%, 3.0% and 2.3%, respectively. The most common multimorbidity combination was generated by the two most common chronic diseases of respiratory disease and cardiovascular disease. Overall, 4.7% of study participants with a mean age of 54 years had multimorbidity and tended to lead less healthy lives.
People with multimorbidity reported more physical inactivity, inadequate sleep, and chronic stress with ORs of 1.2, 1.7, and 2.1, respectively. Multimorbid individuals were current smokers, watched television, and consumed less alcohol.
No association was observed between food quality and morbidity.
Final message The study findings indicate that inadequate sleep and chronic stress should be considered when developing supportive lifestyle programs for people with multimorbidity. Physical inactivity and smoking were also identified as key lifestyle factors among people with multiple chronic diseases. Additional research is needed to evaluate the impact of each lifestyle component on disease prognosis, design lifestyle therapies for multimorbid patients, and examine the influence of lifestyle interventions on clinical outcomes and quality of life. life. |
















