The Centers for Disease Control and Prevention (CDC) has warned US doctors to be alert for a little-known tick-borne allergic disease that may affect nearly half a million Americans. .
There is growing evidence that the syndrome is triggered by a bite from Amblyomma Americanum , known as the lone star tick , which is common across a wide area of the southern, midwestern, and mid-Atlantic regions of the US. , although other ticks may be involved.
Emerging meat allergy linked to tick bites could affect thousands
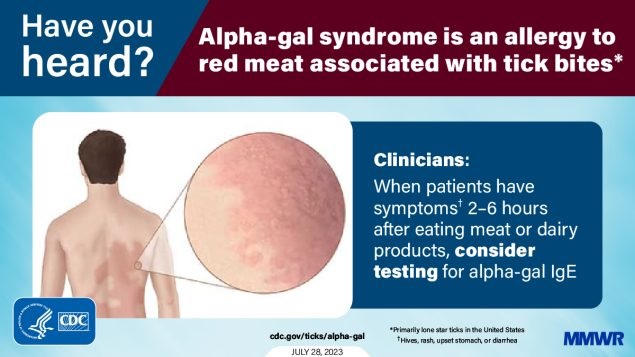
| Alpha-gal syndrome ( AGS) is an emerging immunoglobulin E-mediated allergic condition associated with tick bites that is characterized by a reaction to the oligosaccharide galactose-alpha-1,3-galactose (alpha-gal), which is found in mammalian meat and products derived from mammals, including milk, other dairy products and some pharmaceutical products. Symptoms range from mild (e.g., rash or gastrointestinal upset) to severe (anaphylaxis); Onset usually occurs ≥2 hours after exposure to alpha-gal. There is currently no treatment or cure available. Despite the possible life-threatening reactions associated with AGS, most patients perceive that healthcare providers (HCPs) have little or no knowledge about AGS. |
CDC statement
The CDC reports that between 2010 and 2022, more than 110,000 suspected cases of alpha-gal syndrome were identified . However, because the diagnosis of alpha-gal syndrome requires a positive diagnostic test and clinical examination, and some people with alpha-gal syndrome may not be tested, it is estimated that up to 450,000 people may have been affected. by AGS in the United States, according to two reports issued by the CDC in the Morbidity and Mortality Weekly Report. Studies show that many healthcare providers in the United States are unfamiliar with an emerging and life-threatening allergic condition called alpha-gal syndrome (AGS) , also known as tick-bite-associated meat allergy . Of those aware of AGS, knowledge about diagnosis and management is low.
In one study, 1,500 general/family physicians, internists, pediatricians, nurse practitioners (NPs), and physician assistants (PAs) across the country were surveyed, and results showed that nearly half of respondents had not heard of AGS, about a third reported that they were ’not very confident’ in their ability to diagnose or treat patients with AGS, and five percent felt ’very confident’ in their ability.
In another study, CDC researchers examined laboratory test results from 2017 to 2022 from a laboratory that, as of August 2021, was the largest commercial laboratory offering testing in the United States. Healthcare providers submitted more than 300,000 samples on behalf of patients with suspected clinical suspicion of AGS, and more than 30 percent were positive.
“ Alpha-gal syndrome is a major emerging public health problem, with potentially serious health impacts that can last a lifetime for some patients,” said Dr. Ann Carpenter, epidemiologist and lead author of one of the papers published today. . "It is critical that physicians are aware of AGS so that they can properly evaluate, diagnose and manage their patients and also educate them on tick bite prevention to protect patients from developing this allergic condition."
Alpha-gal is a sugar found in mammalian meat (pork, beef, rabbit, lamb, venison, etc.) and mammalian products (e.g., gelatin, cow’s milk, dairy products, some pharmaceutical products).
Alpha-gal syndrome (AGS), is a serious allergic condition that some people experience after consuming foods or products containing alpha-gal.
There is increasing evidence to suggest that AGS is primarily associated with the bite of a lone star tick in the United States, but other types of ticks have not been ruled out. Localities in the South, Midwest and Mid-Atlantic regions of the United States identified more people who tested positive.
"The burden of alpha-gal syndrome in the United States could be substantial given the large percentage of suspected cases that go undiagnosed due to nonspecific and inconsistent symptoms, challenges in seeking medical care, and lack of medical awareness," said Dr. Johanna Salzer. “It is important for people who think they may have AGS to consult their healthcare provider or an allergist, provide a detailed history of symptoms, have a physical examination, and have a blood test that looks for specific antibodies (proteins produced by your immune system) for alpha-gal.”
People who suffer from AGS may experience a wide range of symptoms, including hives or an itchy rash; nausea or vomiting; heartburn or indigestion; diarrhea; cough; shortness of breath or difficulty breathing; drop in blood pressure; swelling of the lips, throat, tongue or eyelids; dizziness or fainting; or severe stomach pain .
Symptoms commonly appear 2 to 6 hours after eating food or other exposure to products containing alpha-gal (for example, gelatin-coated medications). AGS is diagnosed by an allergist or other healthcare provider and requires a complete history with compatible symptoms and diagnostic testing for specific alpha-gal antibodies. Your healthcare provider may also recommend skin testing for allergies.
Preventing tick bites is important for preventing tick-borne diseases and can reduce your chances of developing AGS.















