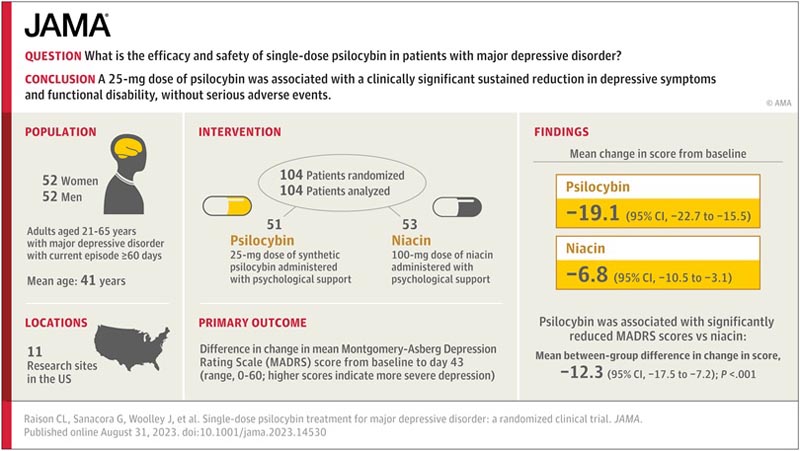
Key points What are the efficacy and safety of psilocybin in patients with major depressive disorder? Findings In a 6-week randomized, placebo-controlled trial in 104 adults, a 25 mg dose of psilocybin administered with psychological support was associated with a rapid and sustained antidepressant effect, measured as change in depressive symptom scores. compared to active placebo. There were no treatment-emergent serious adverse events. Meaning A 25 mg dose of psilocybin was well tolerated and may show promise as a treatment for major depressive disorder when combined with psychological support. |
Importance
Psilocybin shows promise as a treatment for major depressive disorder (MDD).
Aim
To evaluate the magnitude, timing, and durability of the antidepressant effects and safety of a single dose of psilocybin in patients with MDD.
Design, environment and participants
In this Phase 2 trial conducted between December 2019 and June 2022 at 11 research sites in the US, participants were randomly assigned in a 1:1 ratio to receive a single dose of psilocybin versus placebo niacin . administered with psychological support.
Participants were adults aged 21 to 65 years with a Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. diagnosis of MDD of at least 60 days duration and moderate or greater severity of symptoms.
Exclusion criteria included history of psychosis or mania, active substance use disorder, and active suicidal ideation with intent. Participants taking psychotropic agents and otherwise meeting inclusion/exclusion criteria were eligible after medication taper.
Primary and secondary outcomes and adverse events (AEs) were assessed at baseline (conducted within 7 days before administration) and at 2, 8, 15, 29, and 43 days after administration.
Interventions
The interventions consisted of a 25 mg dose of synthetic psilocybin or a 100 mg dose of niacin in identical-appearing capsules, each administered with psychological support.
Main results and measures
The primary outcome was the change in central rater-assessed Montgomery-Asberg Depression Rating Scale (MADRS) score (range, 0-60; higher scores indicate more severe depression) from baseline to baseline. day 43. The key secondary outcome measure was change in MADRS score from baseline to day 8. Other secondary outcomes were change in Sheehan Disability Scale score from baseline to day 43 and sustained response and remission defined by MADRS.
Participants, study site personnel, study sponsor, outcome assessors (evaluators), and statisticians were blinded to treatment assignment.
Results
A total of 104 participants (mean [SD] age, 41.1 [11.3] years; 52 [50%] women) were randomized (51 to the psilocybin group and 53 to the niacin group).
Psilocybin treatment was associated with significantly reduced MADRS scores compared with niacin from baseline to day 43 (mean difference, -12.3 [95% CI, -17.5 to -7.2]; P <0.001) and from baseline to day 8 (mean difference, −12.0 [95% CI, −16.6 to −7.4]; p < 0.001).
Psilocybin treatment was also associated with significantly reduced scores on the Sheehan Disability Scale compared with niacin (mean difference, −2.31 [95% CI, 3.50-1.11]; P < 0.001 ) from the beginning to day 43.
More participants who received psilocybin had a sustained response (but not remission) than those who received niacin.
There were no treatment-emergent serious adverse events (AEs); however, psilocybin treatment was associated with a higher rate of overall AEs and a higher rate of serious AEs.
Conclusions and relevance Psilocybin treatment was associated with a clinically significant sustained reduction in depressive symptoms and functional disability, without serious adverse events. These findings add to growing evidence that psilocybin, when administered with psychological support, may hold promise as a new intervention for major depressive disorder (MDD). |
Trial Registration ClinicalTrials.gov Identifier: NCT03866174















