Diabetic retinopathy ( DR) is one of the most common complications of diabetes and remains the leading cause of preventable blindness in the working-age population. Currently, the global prevalence of this complication remains high, affecting 2 in 10 patients with diabetes, and is expected to remain high until 2045, especially among countries in the Middle East, North Africa and the Western Pacific.
Poor glycemic control and high blood pressure are the main modifiable risk factors to reduce the development and progression of diabetic retinopathy (DR). However, rapid improvement in hyperglycemia may also be a risk factor for DR progression. Early worsening DR (EWDR) was observed in 13.1% of 711 patients with type 1 diabetes assigned to intensive treatment in the Diabetes Control And Complications Trial (DCCT) at 6 and/or 12 months compared to 7.6% of 728 patients assigned to conventional treatment (odds ratio [OR], 2.06; P < 0.001). A similar phenomenon was reported in subjects with type 2 diabetes after rapid improvement in blood glucose levels when switched from oral agents or diet alone to insulin therapy.
The main variables that explain early worsening of DR (EWDR) are the magnitude of the reduction in HbA 1c and the presence of pre-existing diabetic retinopathy (DR). Regarding the first, it should be particularly relevant when HbA 1c is reduced >1.5% in 3 months or >2% in 6 months.
Therefore, the greater the reduction in HbA 1c, the greater the risk of EWDR. Notably, although this reduction usually occurs after treatment with a highly effective antidiabetic drug, EWDR has also been reported after bariatric surgery. This observation points to the reduction of blood glucose levels, rather than any particular antidiabetic agent, as the main reason implicated in EWDR.
However, the possible association between glucagon-like peptide-1 receptor agonists (GLP-1RA) (particularly semaglutide) and early worsening of DR is still under debate. The presence of DR is also an essential risk factor for EWDR. However, the influence of the degree of DR remains to be elucidated. This is because most studies have included subjects without data on DR staging.
On this basis, the aim of the present study is to evaluate, in a nested case-control study , whether EWDR is also a problem in type 2 diabetes patients with mild or moderate non-proliferative DR (NPDR), who represent the vast majority of patients treated in primary care. In addition, the relationship between EWDR and different antidiabetic drugs was also analyzed.
Aim
Early worsening diabetic retinopathy (EWDR) due to rapid decline in blood glucose levels is a concern in diabetes treatment. The objective of the present study is to evaluate whether this is an important issue in subjects with type 2 diabetes with mild or moderate non-proliferative DR (NPRD), who represent the vast majority of subjects with DR seen in primary care.
Methods
This is a retrospective nested case-control study of subjects with type 2 diabetes and prior mild or moderate nonproliferative DR (NPRD). Using the SIDIAP database (“Sistema d’informació pel Desenvolupament de la Recerca a Atenció Primària”), we selected 1,150 individuals with non-proliferative DR (RDNP) and 1,150 matched control subjects (RD without RDNP). The main variable analyzed was the magnitude of the reduction in HbA 1c in the previous 12 months. HbA 1c reduction was categorized as rapid (>1.5% reduction in <12 months) or very rapid (>2% in <6 months).
Results
We did not find any significant difference in HbA 1c reduction between case and control subjects (0.13 ± 1.21 vs. 0.21 ± 1.18; P = 0.12).
The reduction in HbA 1c did not show a significant association with worsening of DR, neither in the unadjusted analyzes nor in the adjusted statistical models that included the main confounding variables: duration of diabetes, baseline HbA 1c, presence of hypertension and antidiabetic drugs.
Furthermore, when stratification was performed by baseline HbA 1c, we did not find that those patients with higher levels of HbA 1c presented a greater risk of EWDR.
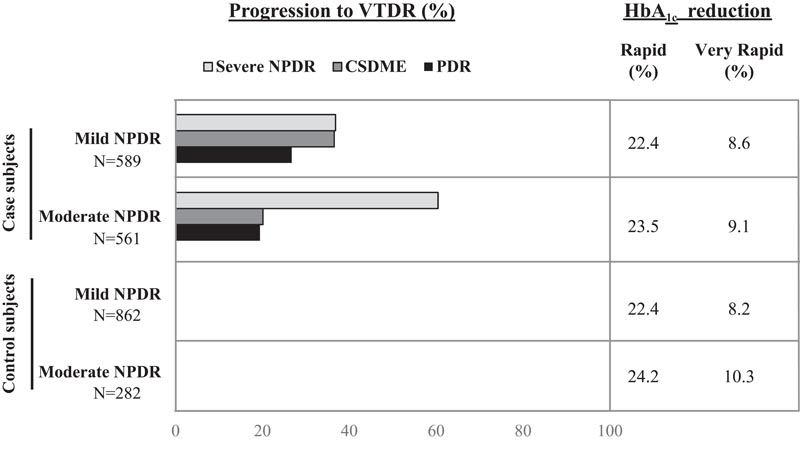
Figure : Progression from mild and moderate NPDR to VTDR according to HbA 1c reduction (rapid and very rapid).
Conclusions Our results suggest that rapid reduction in HbA 1c is not associated with progression of mild or moderate early worsening diabetic retinopathy (EWDR). In summary , clinicians should not be afraid to optimize blood glucose in a relatively short period of time in those subjects with mild or moderate nonproliferative DR (NPRD). However, this strategy cannot be extended to vision-threatening DR, in which careful lowering of HbA 1c should be planned. Therefore, the presence and degree of DR is relevant information that should be available before initiating an intensive glucose-lowering approach. |