According to a study, blood pressure should be measured in both arms and the highest reading should be adopted to improve the diagnosis and treatment of hypertension.
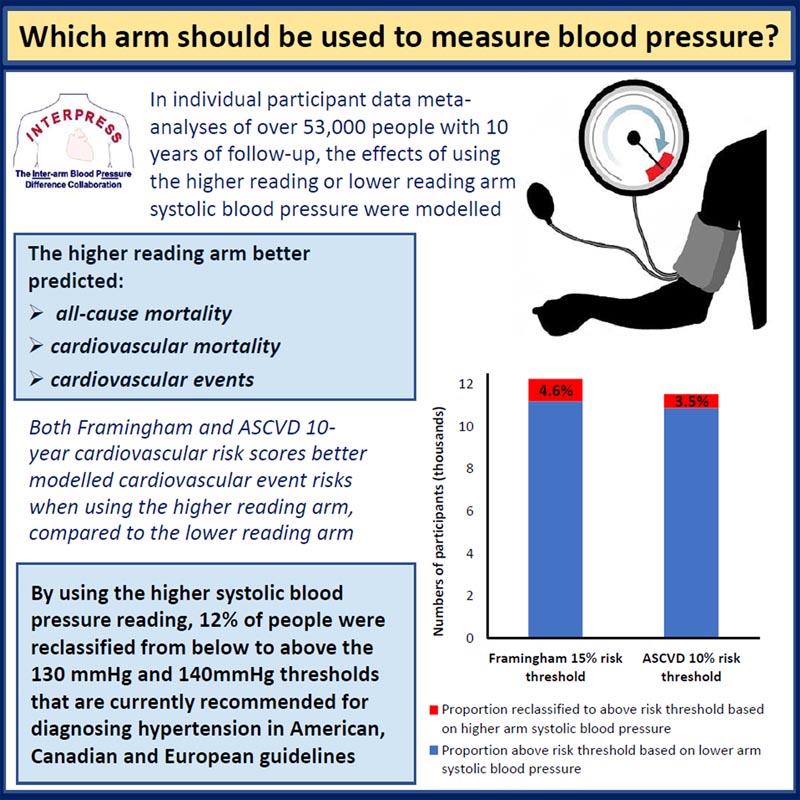
Upper Arm Versus Lower Arm Systolic Blood Pressure and Cardiovascular Outcomes: A Meta-Analysis of Individual Participant Data from the INTERPRESS-IPD Collaboration Background: Guidelines recommend measuring blood pressure (BP) in both arms, adopting the readings from the higher arm for diagnosis and treatment. There is a lack of data to support this recommendation. We assessed the associations of upper and lower arm systolic blood pressure with diagnostic and treatment thresholds, and prognosis of hypertension, using inter-arm blood pressure difference data: individual participant data collaboration. Methods: One-stage multivariable Cox regression models, stratified by study, were used to examine the associations of higher or lower BP in the reading arm with cardiovascular mortality, all-cause mortality, and cardiovascular events, in meta-analyses. of pooled individual participant data from 23 cohorts. Cardiovascular events were modeled for Framingham and atherosclerotic cardiovascular disease risk scores. Model fit was compared using Akaike’s information criteria. Reclassified proportions were also compared between guideline-recommended intervention thresholds. Results: We analyzed 53,172 participants : average age 60 years; 48% women. Upper arm blood pressure , compared with lower arm blood pressure, reclassified 12% of participants at systolic BP thresholds of 130 or 140 mm Hg (both P < 0.001). Upper arm BP models fit best for all-cause mortality, cardiovascular mortality, and cardiovascular events (all P < 0.001). Upper arm BP models best predicted cardiovascular events with Framingham and atherosclerotic cardiovascular disease risk scores (both P < 0.001) and reclassified 4.6% and 3.5% of participants, respectively, into categories higher risk compared to lower arm PAs). Conclusions: Using blood pressure from higher rather than lower reading arms reclassified 12% of people above the thresholds used to diagnose hypertension. All prediction models performed better when upper arm BP was used. Both arms should be measured for accurate diagnosis and treatment of hypertension. Study registration: URL: https://www.clinicaltrials.gov; Unique identifier: CRD42015031227. |
Comments
The research, led by the University of Exeter, analyzed data from 53,172 participants in 23 studies around the world to examine the implications of choosing higher or lower arm pressure.
The study, published in Hypertension , found that using the blood pressure reading from the arm with the highest recording reclassified 12 percent of people as hypertensive, who would have fallen below the diagnostic threshold if the reading had been used. of the lower arm.
Although international guidelines recommend monitoring blood pressure in both arms, the practice is not currently widely adopted in clinics.
Study leader Dr Christopher Clark, from the University of Exeter, said: "High blood pressure is a global problem and poor management can be fatal. This study shows that not measuring both arms and using the reading arm higher will not only result in underdiagnosis and undertreatment of high blood pressure, but also underestimation of cardiovascular risks for millions of people worldwide."
The team found that using the measurement from the higher BP arm compared to using the lower BP arm resulted in 6,572 (12.4%) participants’ systolic blood pressure being reclassified from low to high. from 130 mm Hg, and 6339 (11.9%) from less to more than 140 mm. Hg, placing them above the diagnostic thresholds commonly used for hypertension.
Dr Clark continued: "It is impossible to predict which arm is best for measuring blood pressure as some people have a higher reading on the left arm than the right and in equal numbers the opposite is true. Therefore, "It is important to check both arms to detect high blood pressure correctly. It is a vital step in giving the right treatment to the right people."
"Our study now provides the first evidence that a higher blood pressure reading in one arm is a better predictor of future cardiovascular risk."
The study also revealed that higher arm blood pressure readings better predicted all-cause mortality, cardiovascular mortality, and cardiovascular events, compared to the lower arm reading. The authors highlighted the importance of evaluating both arms in the diagnosis and treatment of hypertension and cardiovascular diseases.
Novelty and relevance
What’s new?
The guidelines recommend adoption of the higher BP arm reading for the diagnosis and treatment of hypertension, based on expert opinion. We studied data from more than 53,000 participants from 23 studies around the world to examine the implications of choosing higher or lower arm blood pressure.
Higher upper arm blood pressure better predicts all-cause mortality, cardiovascular mortality, and cardiovascular events compared with lower arm reading.
Up to 12% of people classified as hypertensive fall below the recommended thresholds for the diagnosis and treatment of hypertension if the lower, rather than the upper, reading arm is used.
What is most relevant?
Routine adoption of upper arm blood pressure measurement allows for better prediction and classification of cardiovascular risk, as well as more accurate diagnosis and treatment of hypertension.
Clinical/pathophysiological implications?
When considering the diagnosis or treatment of high blood pressure, blood pressure should be measured in both arms and all decisions should be based on the measurement of the arm with the highest reading. Failure to do so risks many millions of people around the world being underdiagnosed and undertreated.
Final message This study provides strong evidence that more than 1 in 10 people were recategorized to require additional treatment using the upper rather than lower reading arm.Blood pressure should be assessed in both arms and readings from the upper reading arm should be used in the diagnosis and treatment of hypertension and cardiovascular disease. This choice also significantly improved the prognostic ability of blood pressure measurement for cardiovascular events. Failure to use the highest reading arm risks underdiagnosis, undertreatment of high blood pressure, and underestimation of cardiovascular risk for many millions of people worldwide, missing opportunities to appropriately scale up primary prevention of the diseases. cardiovascular diseases. |
















