Hypertension is the most important modifiable risk factor for morbidity and mortality worldwide.
Lifestyle changes are the cornerstone of prevention and treatment and both governments and industry are instrumental in supporting and implementing these modifications. Additionally, lifestyle changes can not only reduce and control blood pressure (BP), but also improve cardiovascular and general health.
Importantly, well-known lifestyle interventions such as dietary change, alcohol moderation, smoking cessation, and aerobic exercise have now been extended to less obvious strategies such as stress reduction, isometric exercise and reducing exposure to pollution.
Although lifestyle changes are effective, they remain difficult to implement and maintain long-term because many people live in environments that are not conducive. Additionally, doctors are often poorly trained to help patients adopt healthy behaviors.
In the present article, the authors review the updated evidence supporting the use of lifestyle interventions in patients with high blood pressure or people at risk of developing it.
| General recommendation |
Lifestyle goals (summarized in Figure 1) are recommended to prevent or delay the onset of elevated BP and reduce the risk of CVD. Lifestyle modifications should be the first line of antihypertensive treatment in grade 1 hypertension. However, if BP control is not achieved with these changes alone, the authors suggest a combination of lifestyle modifications and antihypertensive medications, since the former improve the effect of pharmacological treatment.
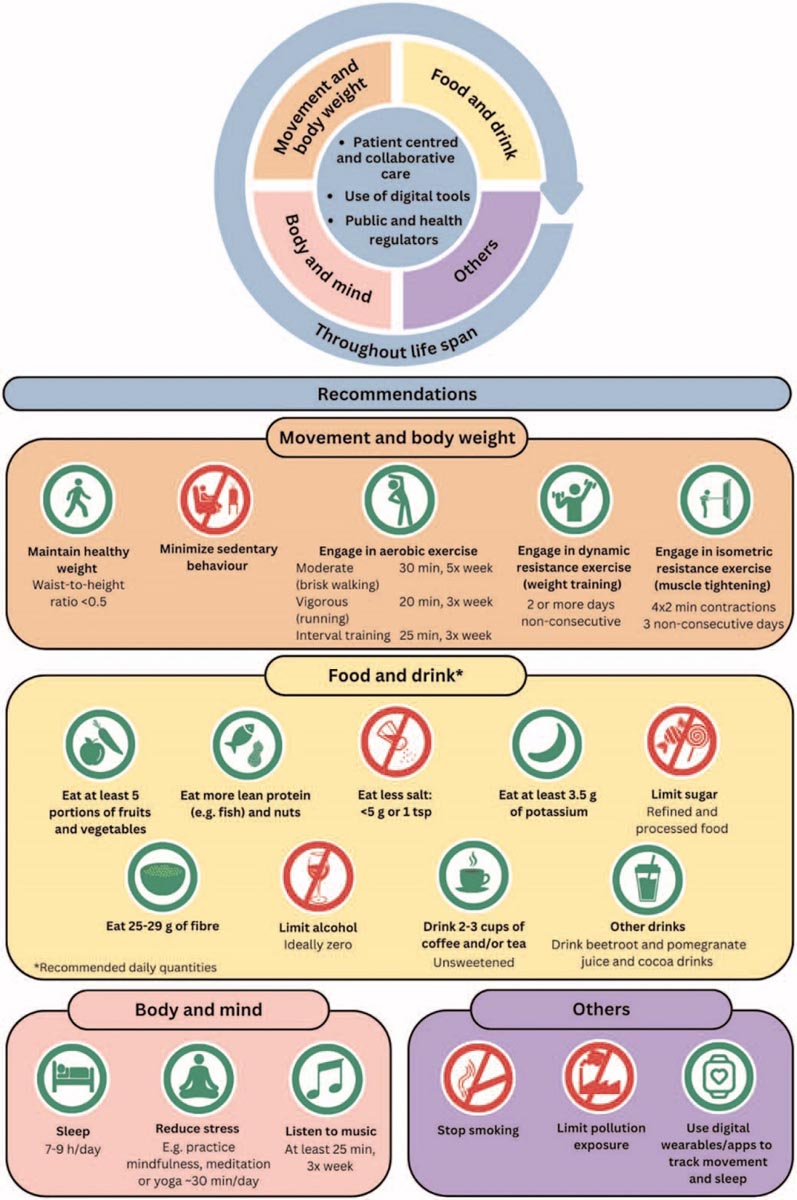
FIGURE 1 . Changes in lifestyle. In green are changes that should be encouraged, increased and respected, for example, the consumption of dietary fiber, improving sleep habits, increasing exercise and adopting mindfulness strategies. In red are the changes to reduce or avoid, for example, the consumption of tobacco and alcohol, a sedentary lifestyle, the consumption of refined sugars and exposure to salt and pollution.
| Weight control |
| Recommendations: |
1. Weight loss should be incorporated into daily life, that is, increasing incidental exercise, walking or cycling more, or playing sports regularly, sitting for less hours, etc. 2. Emphasis should be placed on early intervention and health education programs to maintain a healthy weight throughout life. 3. For people with hypertension, modest weight loss that can be maintained over a long period of time along with a reduction in calorie intake is recommended. 4. Weight loss interventions should be based on cognitive-behavioral strategies (e.g., appetite awareness training, a self-management strategy in which individuals learn to identify internal cues of moderate hunger and satiety and use these cues to guide your eating behavior). 5. Abdominal obesity must be controlled. Ethnic-specific cutoffs for body mass index and waist circumference should be used. 6. The type of weight loss program chosen must be adapted, considering the individual initial weight, age, sex, comorbidities and situational context with the support of a nutritionist. 7. The use of innovative approaches based on behavior change technologies (e.g., apps, text messages) is encouraged for all people with overweight or obesity. |
| Physical activity |
| Recommendations: |
1. All people should be encouraged to engage in physical activity to prevent or control hypertension and cardiovascular diseases. 2. Emphasis should be placed on early intervention (from childhood) and health education programs to maintain physical activity throughout life. 3. Both aerobic and dynamic resistance exercise or their combinations can be used in the prevention and treatment of hypertension and cardiovascular diseases. 4. Adults should get 150 to 300 minutes of moderate-intensity exercise or 75 to 150 minutes of vigorous exercise, or an equivalent combination, weekly. 5. The type of activity/exercise chosen should be individually adapted, considering initial physical status, comorbidities, pharmacological treatment, situational context and be progressive in nature (i.e. start slowly and gradually increase the amount/intensity of activity ). |
| General nutrition |
A-Sal
| Recommendation: |
| 1. Intake of less than 2 g of sodium (-5 g of salt or one teaspoon) per day. |
B-Potassium
| Recommendations: |
1. The European Food and Safety Administration and the WHO recommend a potassium intake of more than 3.5 g per day for adults, while the Academies National Science and Medicine recommend an intake of more than 4.7 g per day for adults. 2. It is necessary to consider individual food and nutritional needs due to the lower body composition between sexes and the greater differences between body mass within and between populations. |
C-Sugar
| Recommendation: |
| 1.Reduce or limit sugar intake both in raw form and in processed foods, drinks and sweets. |
D-Fiber
| Recommendation: |
| 1. Fiber intake of 25 to 29 g/day conferred the greatest risk reduction, but dose-response data suggested that more than 30 g/day conferred additional benefits. |
E-Alcohol
| Recommendations: |
1. Alcohol consumption should be zero to obtain better cardiovascular results. However, the recommended maximum daily limit of alcohol consumption is two standard drinks for men and 1 for women (10 g alcohol/standard drink), although it is recognized that there is no safe limit of alcohol consumption to prevent hypertension. and adverse cardiovascular outcomes. 2. Binge drinking should be avoided. |
F. Non-alcoholic beverages
| Recommendations: |
1. Regular moderate coffee consumption (three to four cups per day) does not negatively affect blood pressure or the cardiovascular system and may be moderately beneficial. 2. The addition of drinks rich in nitrates, such as beet juice, pomegranate juice and cocoa, may be considered. |
| intermittent fasting |
| Recommendations: |
1. Intermittent fasting with calorie restrictions may be beneficial for weight loss and lowering blood pressure, but it is not superior to a general calorie-restricted diet. Therefore, the use of intermittent fasting should depend on patient preference and other considerations. 2. Fasting, even during Ramadan or Lent, is generally safe in low- to moderate-risk populations. |
| Stress reduction |
| Recommendations: |
1. Practice stress reduction techniques at least 3 hours per week to reduce mental stress and BP. 2. Alternatively, practice activities such as yoga, meditation or tai chi for at least 45 minutes a day. 3. Listen to music once a day to three times a week for at least 25 minutes. |
| Sleep |
| Recommendations: |
1. Weight management should be considered to improve sleep quality and treatment of sleep disorders (especially OSA). 2. Sleep hygiene should be addressed and implemented routinely. A sleep duration of 7 to 9 hours per night is recommended for adults. 3. Sleep hygiene approaches include a suitable sleeping environment, regular sleep schedules, sleep routine to prepare for sleep, avoidance of food, caffeine, alcohol and cigarettes around bedtime and at night. exposure to bright light and exercise during the day and its restriction before bed. 4. Stimulus control and building a strong association between bed/bedroom and sleep should be implemented: go to bed only when you are sleepy; establish a sleep routine; apply the 20 minute rule (i.e. if you can’t fall asleep within 20 minutes, get up and go to another room and do non-stimulating activities). 5. Daytime naps longer than 30 minutes should not be routinely recommended, given their effects on sleep pressure and nighttime sleep and the lack of evidence of long-term results. 6. Shift workers may need an individualized approach to developing sleep-wake patterns. Ambulatory BP monitoring should be considered for diagnosis and follow-up evaluations to evaluate nocturnal BP patterns. 7. Screening for sleep disorders (particularly OSA) should be performed in resistant hypertension, in patients with nocturnal hypertension and/or abnormal BP drops. If appropriate, treatment should be implemented, focusing on lifestyle changes and the use of specific treatments (CPAP, oral appliances) to support good sleep habits. 8. People with known sleep disorders (snoring, OSA, insomnia, etc.) should undergo regular BP measurements. Ambulatory BP monitoring should be considered for evaluation of the nocturnal pattern. |
| Smoke |
| Recommendations: |
1.It is strongly recommended to quit smoking (including electronic cigarettes) for its well-established health benefits. Importantly, strategies and approaches must be implemented to prevent weight gain after quitting smoking. 2.Key target populations are those already exposed to smoking and those not yet exposed, largely composed of younger generations. 3.Brief intervention counseling and motivational interviewing techniques in health centers have been shown to be very effective in smoking cessation. |
| Exposure to pollution |
| Recommendations: |
1. Exercise in parks and gardens away from busy roads. 2. Limit time spent outdoors during periods of high pollution. 3. Avoid inefficient burning of biomass for domestic heating. 4. Consider the use of filtration ventilation systems for homes in high pollution areas. |
| Over-the-counter medications and nutritional supplements |
| Recommendations: |
1. The intake of vitamins, minerals and micronutrients should be obtained as part of a healthy, nutrient-rich and balanced diet. 2. Health supplements do not replace a balanced diet and are not recommended as a treatment for hypertension. |
| Behavioral interventions and digital health |
| Recommendations: |
1. Healthcare providers should be trained in behavior change approaches and digital assistive technologies to facilitate action and control hypertension. 2. Behavioral changes should be comprehensive and encompass improvement and maintenance of oral hygiene to prevent periodontitis and improve BP control. 3. Continued use of validated wearable devices and digital tools to improve symptom awareness, introduce potential reminders (e.g. for medication intake or promote increased incidental exercise), assist behavior change (e.g. establishment of objectives, decision support, self-monitoring, which can integrate portable data, Reminder and alert systems, digital support conversational agents should be encouraged to improve user adherence, motivation and self-efficacy, intervention personalization programming). 4. Introduce communication technologies to facilitate guidance and professional input or social support (digital spaces to communicate with healthcare providers or peers, SMS messages) as a stand-alone digital intervention or integrated into a multicomponent intervention. |
| Holistic approach |
| Recommendations: |
1. Implementation of comprehensive patient care, as evidenced in Latin America, Canada and some African countries, to provide optimal treatment and management of BP. 2. Improve access to diagnosis, treatment and management of BP in regional and rural areas. |
| Overview and a look at the future of assisted lifestyle interventions |
This document presents recommendations that support a healthy lifestyle to control and maintain adequate blood pressure: more exercise, less salt, sugar and saturated fat in the diet, more fruits, vegetables and dietary fiber, no smoking or alcohol.
Emerging evidence of newer modalities was also presented and the potential for greater use of digital technologies to help improve lifestyle habits in a personalized way was discussed. In fact, there are many mobile phone “apps” that can be used to help track movement, diet, and habits. These technologies can be used to monitor weight, evaluate meal composition and calorie content.
Importantly, data supporting many of these breakthrough interventions are sparse and larger studies are essential to evaluate effectiveness.