As COVID-19, caused by SARS-CoV-2, spreads around the world, diverse patterns of associated dermatological diseases continue to emerge. Early reports classified multiple cutaneous manifestations of SARS-CoV-2 infection. In this article, we report the observation of a recent associated mucocutaneous rash in a pediatric patient with confirmed SARS-CoV-2 infection.
A previously healthy 17-year-old male presented to the emergency room with 3 days of mouth pain and painless penile erosions. A week earlier, he experienced transient anosmia and ageusia that had since resolved spontaneously.
At that time, he was tested for SARS-CoV-2 infection using nasopharyngeal polymerase chain reaction (PCR), the results of which were positive. He denied fever, cough, dyspnea, rhinorrhea, and gastrointestinal symptoms at any time. Although he had taken acetaminophen and ibuprofen before presenting to the emergency department, he took no medications prior to the onset of the mucocutaneous rash. The patient had no fever and was not in danger.
His vital signs were normal, including a respiratory rate of 16 breaths per minute and an oxygen saturation of 97%.
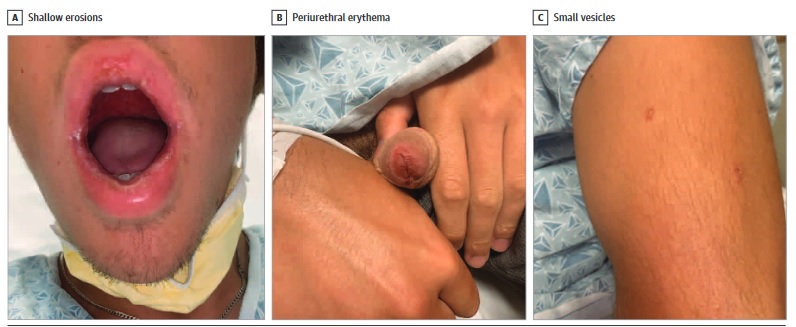
The physical examination revealed superficial erosions of the vermilion lips and hard palate, circumferential erythematous erosions of the periurethral glans of the penis, and 5 small vesicles on the trunk and upper extremities (Figure 1). The remainder of the mucocutaneous (including palms and soles), cervical lymphatic, and cardiopulmonary examinations was unremarkable.
Laboratory test results revealed a normal white blood cell count (7030 leukocytes/μL [to convert to × 109/L, multiply by 0.001]; reference: 5240-9740 leukocytes/μL) with mild absolute lymphopenia (930 lymphocytes/μL). μL; reference: 1030 -2180), slightly elevated creatinine level (1.2 mg/dL [to convert to μmol/L, multiply by 88.4]; reference: 0.3-1.0 mg/dL), normal liver function, slightly elevated C-reactive protein level (3.0 mg/dL [to convert to mg/L, multilayer by 10]; reference: <0.5 mg/dL), normal D-dimer level (0.37μg/mL [to convert to nmol/L, multiply by 5,476]; reference: <0.5 mg/dL) and normal ferritin level (180 ng/mL [to convert to μg/L, multiply by 1]; reference: 10- 320 μg/L).
Microbiological test results revealed repeat positive SARS-CoV-2 nasopharyngeal PCR and negative nasopharyngeal PCR tests for Mycoplasma pneumoniae, adenovirus, Chlamydo-phila pneumoniae, human metapneumovirus, influenza A/B, parainfluenza 1 to 4, rhinovirus and viruses syncytial respiratory. Titers of Mycoplasma pneumoniae IgM levels were negative, but Mycoplasma pneumoniae IgG levels were elevated.
A diagnosis of reactive infectious mucocutaneous eruption (RIME) associated with SARS-CoV-2 was made, and betamethasone valerate 0.1%, lip and penis ointment, intraoral dexamethasone solution, viscous lidocaine, acetaminophen and ibuprofen were prescribed.
However, he noted progressive worsening of oral pain over the next 3 days, prompting initiation of oral prednisone, 60 mg (approximately 1 mg/kg), daily for 4 consecutive days (Figure 2A).
This was followed by a drastic improvement of hismucositis (Figure 2B). He had a brief recurrence of oral mucositis 3 months later, but this also resolved quickly with pred-nisone, 80 mg, for 6 days.

Discussion
Previously known as mycoplasma-induced rash and mucositis, RIME has emerged as the preferred terminology to include mucocutaneous eruptions that are caused by other infectious agents.2 This case describes RIME secondary to SARS-CoV-2 infection, details its resolution with systemic steroids , and points out the possibility of recurrence with milder subsequent symptoms, as previously reported.
The combination of anosmia and ageusia, multiple positive SARS-CoV-2 PCR tests, and no other contemporary infections identified (the high titer of Mycoplasma pneumoniaeIgG with a low titer of IgM and a negative nasopharyngeal PCR likely indicated prior exposure) suggests that SARS-CoV-2 is the infectious trigger.
The limited skin involvement and absence of dark diagonal lesions also distinguish RIME from Stevens-Johnson syndrome and erythema multiforme (which has been described in association with SARS-CoV-2 infection).
Additionally, RIME can be distinguished from Stevens-Johnson syndrome. The newly described multisystem inflammatory syndrome in children, which is associated with Kawasaki disease-like features, including mucocutaneous involvement, systemic symptoms, and dramatically elevated systemic inflammatory markers.
This case highlights what, to our knowledge, is the first report of CoV-2-induced SARS -RIME and distinguishes this entity from other mucocutaneous eruptions with substantially different prognoses and treatment algorithms.