According to a report from the World Health Organization (WHO), 53% of the Western population consumes alcohol regularly. Today’s drinkers consume an average of 32.8 g of alcohol per day, and the content of a standard drink ranges, depending on the country, from 8 g (for example, the United Kingdom2) to 14 g in the United States and 13, 6 g in Canada to 20 g in Austria.
Atrial fibrillation ( AF) is the most common symptomatic arrhythmia worldwide, and the combination of population aging and lifestyle factors, including alcohol consumption and its consequences, contribute to a growing incidence of this disease ( Figure 1 ).
Although the cardiovascular protective effect of small amounts of alcohol has been discussed, for example, in vascular diseases, moderate levels of habitual consumption may be associated with AF. Consequently, current consensus documents recommend comprehensive management of lifestyle components, including avoidance of excessive alcohol consumption, to prevent the onset and progression of AF.
In this paper, the authors reviewed published reports on alcohol and AF, including pathophysiological mechanisms, role of excessive alcohol consumption, habitual drinking at all levels, links between alcohol and other risk factors for AF and the prognostic or therapeutic implications.
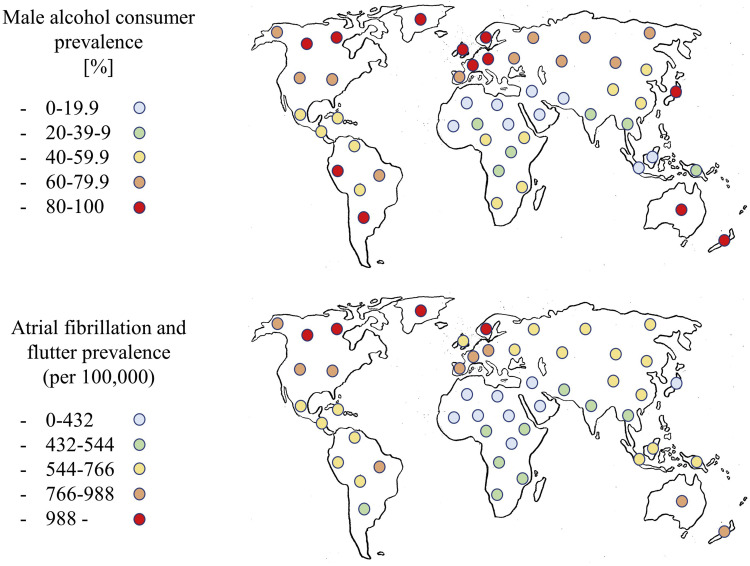
Figure 1. World map: alcohol consumption versus prevalence of atrial arrhythmia. (Above) Male prevalence of alcohol consumption, %. (Bottom) Prevalence of atrial fibrillation and flutter, per 100,000. Of note, this figure represents a graphical illustration to visualize the association between the prevalence of atrial flutter/fibrillation and alcohol consumption, based on the male prevalence of alcohol consumption. This figure does not inform the specific relationships of each country or sex.
| Association between alcohol consumption and AF |
Excessive alcohol consumption and holiday heart syndrome. Vacation heart syndrome was first introduced by Ettinger and colleagues in 1978, who described hospitalization for AF after excessive weekend drinking in 24 patients. Although some of these people consumed alcohol regularly, later research showed that holiday heart syndrome is not unique to habitual drinkers, but can also occur in non-drinkers after an episode of heavy drinking.
It may be difficult to assess a definite temporal relationship between alcohol consumption and the genesis of AF, as some patients develop AF at the time of alcohol ingestion, while others experience AF between 12 and 36 hours after the excessive event. AF usually ends within 24 hours of consumption, but one-third of patients may experience recurrences of AF with subsequent binge eating.
> Habitual alcohol consumption
Regular alcohol consumption may surpass hypertension or obesity as a risk factor for AF. In a Japanese community population-based cohort study (8602 participants), heavy alcohol consumption (>69 g/day) was associated with a hazard ratio (RI) of developing AF of 2.68, compared with RI of 1 .72 for obesity and 1.02 for hypertension.
The relationship between chronic moderate to high alcohol consumption and the incidence of AF is well established, but an increased risk of AF with low or high levels of alcohol consumption has not been consistently demonstrated.
> Specific list of drinks, alcohol and FA
It is not clear how different alcoholic beverages contribute to the risk of AF. Some studies reported that of those who consumed > 14 standard drinks per week, only wine and spirits, and not beer, were associated with an increased risk of AF.
> Specific relationship of sex, alcohol and AF
Some studies showed an increased risk of AF incidence in men who consume alcohol. Several studies failed to show an increased risk of AF at all alcohol levels in women.
> Effect of alcohol withdrawal.
Most current data suggest a relatively linear relationship between alcohol consumption and new-onset AF, and based on observational and non-randomized studies, there is likely no safe level of daily alcohol intake in patients with a history of AF. .
> Alcohol withdrawal syndrome
Sudden cessation of excessive drinking can lead to alcohol withdrawal syndrome (AAS), which is associated with both atrial and ventricular arrhythmia.
| Pathophysiology |
The onset of AF triggers is promoted by alcohol due to increased autonomic imbalance and direct acute atrial electrophysiological effects, resulting in shorter atrial action potentials, greater dispersion of refractoriness, and slower intra-atrial conduction ( Figure 2 ).
Prolonged alcohol consumption facilitates an atrial cardiomyopathy that resembles atrial structural, functional, and electrical remodeling processes, thus stabilizing AF episodes and contributing to their progression.
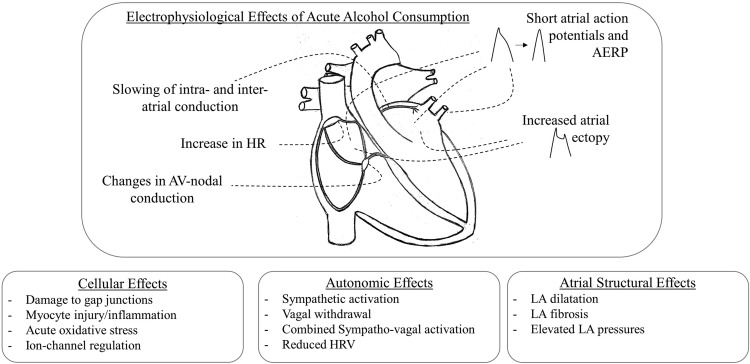
Figure 2 . Arrhythmogenic mechanisms of alcohol. The electrophysiological, cellular, autonomic and atrial structural effects caused by acute alcohol consumption. AERP: atrial effective refractory period; AV, atrioventricular; HR, heart rate; HRV, heart rate variability; LA, left atrium.
> Acute and intermediate arrhythmogenic effects of alcohol consumption
In humans, the acute cardiac effects of alcohol were initially described in 14 patients undergoing electrophysiological examinations. In that study, five standard shots of whiskey caused a shortening of the atrial refractory period and slower intra-atrial conduction. More recently, a publication demonstrated that recent alcohol consumption was associated with an increase in individual episodes of AF in 100 patients equipped with a continuous ECG monitor and a transdermal ethanol sensor placed on the ankle for 4 weeks.
> Atrial cardiomyopathy due to chronic alcohol consumption
Chronic alcohol consumption is associated with atrial cardiomyopathy, reflecting both structural and functional remodeling. in human studies, where AF patients had significantly shorter effective atrial refractory periods and where electroanatomical mapping revealed lower global bipolar voltages, complex atrial potentials, and slow atrial conduction velocity in drinkers compared to non-drinkers.
In humans, alcohol consumption is associated with atrial mechanical dysfunction and alcohol is a predictor of enlarged LA diameter and incident AF. Cardiac MRI in healthy binge drinkers could further shed light on underlying structural changes, because transient increases in ventricular T2 signal intensity were indicative of myocardial edema and global relative enhancement consistent with hyperemia.
> Autonomic effects of alcohol
Alcohol consumption is associated with autonomic activation, resembling both sympathetic and vagal responses. In general, vagal activation shortens atrial refractoriness and may facilitate reentry, while sympathetic activation increases cellular calcium concentrations, which in combination with spontaneous calcium release from the sarcoplasmic reticulum may trigger AF triggers. Furthermore, AF itself can be triggered by the simultaneous discharge of the sympathetic and parasympathetic nervous systems.
> Alcohol consumption and comorbidities associated with AF
AF is often a consequence of atrial cardiomyopathy potentially comprised of a wide range of comorbidities and risk factors associated with AF. Alcohol consumption is pathophysiologically linked to AF risk factors, such as hypertension, sleep apnea, and left ventricular dysfunction, which may perpetuate an AF substrate.
Although alcohol increases the risk of arrhythmia in healthy people, preexisting atrial structural alterations are suspected of having an increasing impact on arrhythmogenesis, which becomes important as chronic alcohol intake induces structural remodeling.
| Conclusion and therapeutic implications |
Alcohol consumption is an accepted and popular component of lifestyle, but excessive consumption, as well as habitual alcohol consumption at moderate levels, are associated with an increased risk of AF through direct effects that transiently increase the risk of AF ( holiday heart syndrome) and the progressive development of an arrhythmogenic substrate.
Although subject to potential confounding, results from epidemiological studies paint a fairly consistent picture that alcohol abstinence is beneficial for the recurrence and treatment of AF and for the prevention or development of associated comorbidities. As the relationship between alcohol consumption and AF risk appears to be fairly linear, there may not be a safe level of daily alcohol intake in patients with a history of AF. However, more studies are needed to support the evidence for the best clinical recommendations.
















