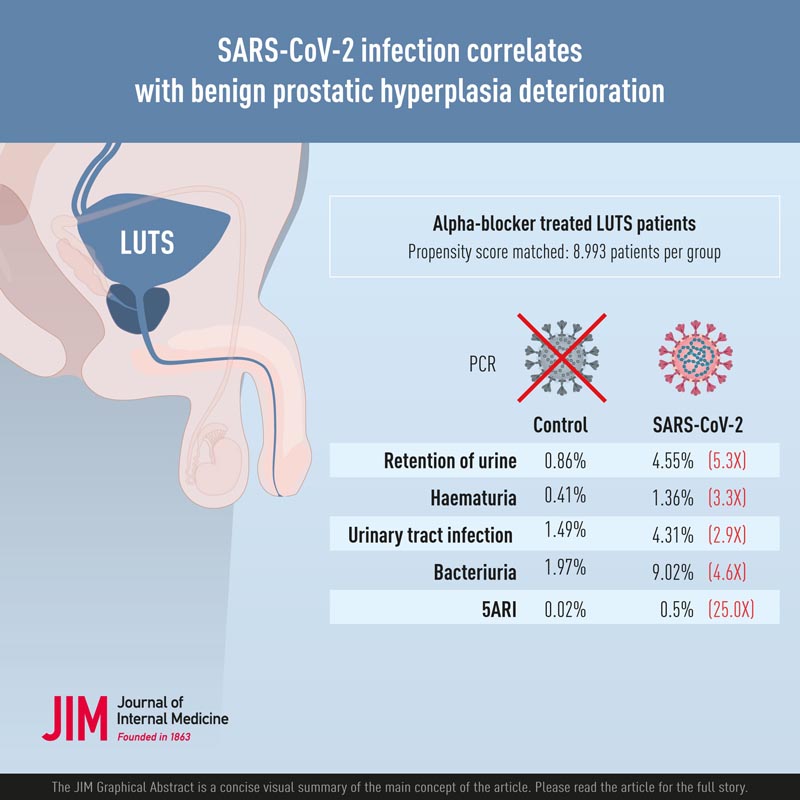
Research published in the Journal of Internal Medicine indicates that SARS-CoV-2 infection can worsen lower urinary tract symptoms (LUTS) in men.
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) affects extrarespiratory systems, and small-scale studies show worsening of male lower urinary tract symptoms (LUTS) after coronavirus disease 2019 (COVID-19). ).
This study explores the correlation between SARS-CoV-2 infection and complications of male benign prostatic hyperplasia (BPH) using large-scale real-world data.
| Materials and methods |
All male patients attending the Hong Kong public health system and receiving alpha-blocker monotherapy for LUTS from 2021 to 2022 were included in this study.
Patients with and without positive polymerase chain reaction (PCR) test for SARS-CoV-2 are selected as exposure group and control group, respectively.
Baseline characteristics are retrieved and propensity score matching is performed to ensure balance of covariates between the two groups. Complications of BPH were then compared and subgroup analyzes were performed.
| Results |
After propensity score matching, 17,986 patients were included for analysis , among whom half had SARS-CoV-2 infection confirmed by PCR (n = 8993).
Compared with controls, the SARS-CoV-2 group demonstrated a statistically significant higher incidence of urine retention (4.55% vs 0.86%, p < 0.001), hematuria (1.36% vs 0. .41%, p < 0.001), clinical urinary symptoms of urinary tract infection (UTI) (4.31% vs 1.49%, p < 0.001), culture-proven bacteriuria (9.02% vs 1. 97%, p < 0.001) and addition of 5ARI (0.50% vs 0.02%, p < 0.001).
Subgroup analysis demonstrated similar differences between different age groups. There are no statistically significant differences in the incidence of retention, hematuria or addition of 5ARI between different severities of COVID-19.
| Conclusions |
| SARS-CoV-2 infection is associated with a higher incidence of urinary retention, hematuria, UTI, and the addition of short-term combination therapy, regardless of COVID-19 severity. This is the largest study demonstrating the detrimental urological effects of SARS-CoV-2 infection. |
| Comments |
The study included 17,986 men who received LUTS medications within the Hong Kong public health system in 2021-2022, half of whom had SARS-CoV-2 infection.
The SARS-CoV-2 group had significantly higher rates of urine retention (4.55% versus 0.86%); blood in urine (1.36% versus 0.41%); clinical urinary tract infection (4.31% versus 1.49%); bacteria in urine (9.02% vs. 1.97%); and adding 5-alpha reductase inhibitors, which are medications prescribed for an enlarged prostate. (0.50% vs. 0.02%).
These urological manifestations occurred regardless of the severity of COVID-19.
The findings could be related to the presence of certain proteins targeted by SARS-CoV-2 that are known to be expressed in the prostate.
"We are excited to be the first to report the effects of COVID-19 on the complications of benign prostatic hyperplasia (or prostate enlargement) and also demonstrate the alarming extent of its urological effects," said corresponding author Alex Qinyang Liu. , MD, from Prince Hospital of Wales in Hong Kong.
| Discussion |
This is the largest cohort study demonstrating that SARS-CoV-2 infection, in male patients receiving medical treatment for baseline lower urinary tract symptoms (LUTS), is associated with a higher incidence of BPH complications in terms of ROU, UTI and hematuria, as well as with the addition of a combination therapy in the SARS-CoV-2 group. This result follows our hypothesis that male patients infected with SARS-CoV-2 are more likely to suffer from LUTS deterioration.
This association is not without biological plausibility, as the co-expression of ACE2 and TMPRSS2 in the prostate makes it a target for SARS-CoV-2, causing inflammation and, therefore, these results of interest. Metabolic dysregulation associated with SARS-CoV-2 infection could have accelerated pathophysiological mechanisms that increase systemic inflammation and oxidative stress , which in turn worsens LUTS.
Furthermore, concomitant psychological and environmental stress during a SARS-CoV-2 infectious episode could also have contributed to lower urinary tract dysfunction. The results show a strong positive correlation suggesting a significant urological manifestation of SARS-CoV-2, with relative risks of BPH complications including ROU, hematuria, clinical UTI and bacteriuria in COVID-19 patients up to 5.31, 3.30, 2.90 and 4.58 respectively.
Given the high infectivity and unprecedented scale of COVID-19, these urological symptoms and complications represent a significant clinical burden that physicians and urologists must be aware of.