Retinal pigment epithelium detachment is anatomically defined as the separation of the retinal pigment epithelium from Bruch’s membrane. These detachments are associated with a series of retinal pathologies, the most common being neovascular age-related macular degeneration (AMD) and has been identified in 63 to 80% of eyes with neovascular AMD.
Currently there are few prospective studies that demonstrate which treatment is effective for pigment epithelial detachment associated with neovascular AMD and without treatment a significant loss of visual acuity occurs in 40 to 50% of eyes within an average period of 9 to 10 months.
Likewise, some studies have observed loss of visual acuity after treatment with anti-vascular endothelial growth factor (anti-VEGF) in eyes with fibrovascular pigment epithelium detachment.
| Patients and methods |
An exhaustive review of the literature was carried out to evaluate the best treatment against retinal pigment epithelium detachment in patients with neovascular AMD, according to previous retrospective and prospective studies on the subject.
Anti-VEGF treatment for neovascular AMD was used in retrospective studies, with ranibizumab, aflibercept and bevacizumab. These studies investigated changes in best-corrected visual acuity and anatomical outcomes (changes in retinal pigment epithelium structure). The results of the studies were diverse without any determined trend.
Five studies found anatomical and visual improvements, another five reported visual stability with anatomical improvements, and one observed visual deterioration despite anatomical improvements.
In general, studies indicate that there is no predictable correlation between anatomical and functional improvement in eyes with pigment epithelial detachment and neovascular AMD, nor can visual improvement be attributed to switching anti-VEGF agents, despite anatomical improvements. .
The conclusions of six prospective studies were analyzed. Taken together, the six prospective studies provide important information on what would be the best treatment for eyes with retinal pigment epithelium detachment and AMD. As in retrospective studies, there was no correlation between reduction in detachment height and improvement in vision.
Prospective studies indicate that there would be no correlation between anatomical and functional response. There could be a difference in the response to anti-VEGF treatment depending on the subtype of neovascularization.
Specifically, certain studies indicate that eyes with NV type E have a better response to treatment, which implies that baseline evaluation of NV subtype using angiography and DE OCT could serve to define the best treatment. There is also a difference in response depending on the subtype of pigment epithelial detachment.
Some studies show a better response to treatment in eyes with serous pigment epithelium detachment.
Finally, studies show greater improvement in vision at 1 or 2 months with dose 2.0 of ranibizumab, but at 12 months there are no significant differences between the groups. Some eyes with fibrovascular PED did not respond to treatment; however, despite not responding, they could have some visual improvement or achieve stability with treatment.
Retinal pigment epithelial tears may occur in 15 to 20% of eyes after treatment with anti-VEGF, especially detachments larger than 500 to 600 µm, however, vision may stabilize with continued treatment. Atrophy may complicate eyes with pigment epithelial detachment and neovascular AMD following anti-VEGF treatment, especially associated with complete resolution of the detachment.
The illustration shows a tear that developed after several injections of anti-VEGF. A) The characteristic form of tear is observed in the fundus image (red arrow). B) The tear can also be seen on OCT (red arrow).
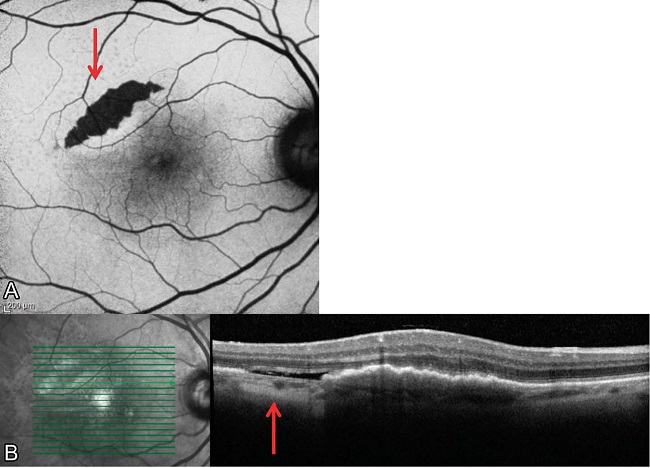
The tear was reduced after several years and many injections of anti-FCEV. With continuous treatment the patient was able to maintain visual acuity at 20/40 in the affected eye.
















