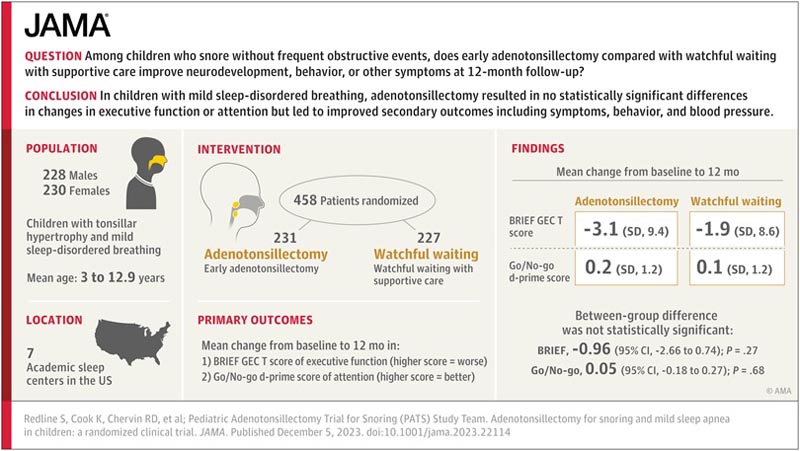
Key points Among children who snore without frequent obstructive events, does early adenotonsillectomy, compared with watchful waiting with supportive care, improve neurodevelopment, behavior, or other symptoms at 12-month follow-up? Findings In this randomized clinical trial of 458 children with mild sleep-disordered breathing (SDB), adenotonsillectomy compared with watchful waiting produced no significant differences in executive function or attention at 12 months. The adenotonsillectomy group improved quality of life, symptoms, behavior, and blood pressure, which were among the secondary outcomes measured. Meaning In children with mild sleep-disordered breathing, adenotonsillectomy did not produce statistically significant differences in changes in executive function or attention, but led to improved secondary outcomes, including symptoms, behavior, and blood pressure. |
Summary
Importance
The usefulness of adenotonsillectomy in children who snore habitually without frequent obstructive breathing episodes (mild sleep-disordered breathing [SDB]) is unknown.
Goals
To evaluate early adenotonsillectomy compared with watchful waiting and supportive care (watchful waiting) on neurodevelopmental, behavioral, health, and polysomnographic outcomes in children with mild sleep-disordered breathing.
Design, environment and participants
Randomized clinical trial enrolling 459 children ages 3 to 12.9 years with snoring and an obstructive apnea-hypopnea index (AHI) less than 3 enrolled at 7 US academic sleep centers since June 29, 2016 until February 1, 2021. and follow-up for 12 months.
Intervention
Participants were randomized 1:1 to early adenotonsillectomy (n = 231) or watchful waiting (n = 228).
Main results and measures
The 2 primary outcomes were changes from baseline to 12 months for the caregiver-reported Behavioral Rating Inventory of Executive Function (BRIEF) Global Executive Composite (GEC) T-score, a measure of executive function; and a computerized test of attention, the Go/No-go (GNG) test d-prime signal detection score, which reflects the probability of responding to target versus nontarget stimuli.
Twenty-two secondary outcomes included 12-month changes in neurodevelopment, behavior, quality of life, sleep, and health outcomes.
Results
Of the 458 participants in the analyzed sample (231 adenotonsillectomy and 237 expectant management; mean age, 6.1 years; 230 women [50%]; 123 blacks/African Americans [26.9%]; 75 Hispanics [16.3%] ; median AHI, 0.5 [IQR, 0.2-1.1]), 394 children (86%) completed the 12-month follow-up visits.
There was no statistically significant difference in change from baseline between the 2 groups in executive function (BRIEF GEC T scores: −3.1 for adenotonsillectomy vs −1.9 for watchful waiting; difference, −0.96 [CI 95%, −2.66 to 0.74]) or attention (GNG d-prime scores: 0.2 for adenotonsillectomy vs. 0.1 for watchful waiting; difference, 0.05 [95% CI, −0. 18 to 0.27]) at 12 months.
Behavioral problems, sleepiness, symptoms, and quality of life improved more with adenotonsillectomy than with watchful waiting.
Adenotonsillectomy was associated with a greater decrease at 12 months in systolic and diastolic blood pressure percentile levels (difference in changes, −9.02 [97% CI, −15.49 to −2.54] and − 6.52 [97% CI: −11.59 to −1.45], respectively) and less progression of AHI to more than 3 events/h (1.3% of children in the adenotonsillectomy group compared to 13.2% in the watchful waiting group; difference, -11.2% [97% CI, -17.5% to - 4.9%]). Six children (2.7%) experienced a serious adverse event associated with adenotonsillectomy.
Conclusions
Removal of tonsils and adenoids improved sleep quality and some behavioral problems in children with mild sleep apnea
The surgery did not improve children’s neurodevelopmental functioning but was associated with better quality of life, sleep symptoms and blood pressure 12 months after surgery, according to a randomized control trial led by researchers at Brigham and Women’s Hospital. and Harvard Pilgrim Health Care Institute.
In children with mild sleep-disordered breathing, adenotonsillectomy, compared with watchful waiting, did not significantly improve executive function or attention at 12 months.
However, children with adenotonsillectomy had better secondary outcomes, including behavior, symptoms and quality of life, and lower blood pressure, at 12-month follow-up.
Comments
Between 6% and 17% of children suffer from sleep-disordered breathing, characterized by habitual snoring, increased respiratory effort, and sleep apnea. If left untreated, the disorder can put children at increased risk for neurodevelopmental impairment, reduced quality of life, and cardiovascular and metabolic diseases.
Enlarged tonsils are one of the main risk factors for sleep-disordered breathing, and adenotonsillectomy ( surgical removal of the tonsils and adenoid glands) is a first-line treatment for children with this disorder. However, there is limited data to support or refute the benefits of this surgery for children with mild forms of the disease.
In a randomized clinical trial, a team led by researchers at Brigham and Women’s Hospital, a founding member of the Mass General Brigham Health System, in collaboration with the Harvard Pilgrim Health Care Institute, evaluated the effects of early adenotonsillectomy.
The surgery did not make a significant difference in the study’s two primary endpoints: executive function and attention , but it did improve sleep quality, reduce snoring, and was associated with improved behavior and reduced daytime sleepiness in children. with mild sleep disorders. Children who received the surgery also had reduced blood pressure and were less likely to show signs of disease progression compared to children in the control group.
The findings appear in The Journal of the American Medical Association.
"Our data suggest that for children who have no symptoms other than snoring , it is reasonable to monitor them over time without proceeding to surgery ," said first author Susan Redline, MD, MPH, director of Epidemiology Programs in Medicine. of Sleep and Cardiovascular and Sleep Medicine. "On the other hand, for children who have problems with disturbed sleep, daytime sleepiness, and behavioral problems, our data suggest that surgery may be a very reasonable option , even if a sleep study shows that they do not have frequent apneas."
To examine the impact of early adenotonsillectomy on neurodevelopment, sleep quality, behavior, and overall health, researchers conducted a randomized clinical trial in 459 children with mild sleep-disordered breathing (defined as habitual snoring without frequent episodes). of apnea [“breathing pauses”) and enlarged tonsils. The children, half of whom received adenotonsillectomies, ranged in age from 3 to 12.9 years and were enrolled at seven academic sleep centers across the United States. The team collected measurements of sleep quality, cognition, behavior and general health before treatment and during follow-up appointments at 6 and 12 months. Caregivers also completed questionnaires about their children’s social behavior and executive function.
Although adenotonsillectomy did not have a significant impact on measures of neurodevelopmental function, the treatment was associated with improvements in sleep quality and reduction in snoring, and a reduction in behavioral problems, daytime sleepiness, and blood pressure. arterial. Children who received surgery were also less likely to show disease progression: at 12-month follow-up, only 1.3% of children in the adenotonsillectomy group progressed to having more than three apnea events per hour compared with 13.2% of children in the control group.
"We hope that our data will provide evidence to inform future clinical guidelines that help surgeons, pediatricians and sleep physicians practice evidence-based care," Redline said. "And to parents, we hope that doctors can communicate this information in a way that helps you decide, together with your doctor, whether your children should go ahead and have surgery."
Next, the researchers plan to investigate the impact of adenotonsillectomy on healthcare utilization and hope to also investigate the long-term impacts of the surgery. "Our team is very interested in longer-term follow-up of children," Redline said. "There are open questions about the impact of tonsil removal over the course of a child’s life, as well as its impact on growth and development trajectories beyond one year."
Clinical implications
These findings do not support adenotonsillectomy in children with mild SDB with the goal of improving cognition, although differences may have been observed with additional follow-up.
In contrast, surgery improved secondary outcomes including behavior, symptom burden, quality of life, blood pressure, and apnea/hypopnea index (AHI) level over 12 months. The current findings suggest that a low AHI on polysomnography does not exclude the potential benefits of surgery in children with habitual snoring.
The mechanisms by which mild sleep-disordered breathing (MSD) contribute to adverse outcomes are unclear, but may be related to chronic effects of subtle periods of hypoventilation and increased work of breathing, which are not well characterized by AHI level. but they can improve with adenotonsillectomy.
Although children in this study were identified by caregiver-reported snoring and infrequent obstructive events on polysomnography, most had at least an elevated score on several validated mild sleep-disordered breathing (SDB) symptom or behavioral questionnaires. Future research is needed to develop easy-to-use screening instruments to identify which children are most likely to benefit from adenotonsillectomy compared to watchful waiting. There is also a need to identify objective measures that better characterize the physiological stressors that mediate SDB-related health outcomes.
Fragment of the editorial that accompanies the article
Adenotonsillectomy or watchful waiting in patients with pediatric sleep-disordered breathing
Habitual snoring and sleep-disordered breathing (SDB) are remarkably common conditions in children. Lack of sleep has a significant effect on the neurobehavior and quality of life (QoL) of the child and therefore on the parent-child dyad, which exceeds the effect of a prevalent and treatable disease. When considering surgery as a treatment, the surgeon and family balance the potential benefit to the child, the associated morbidity, the related financial burden, and the cost-effectiveness of surgery compared with medical treatment or watchful waiting.
When there is a choice, the collaborative process of shared decision-making between the surgeon, the child, and their family is often used to consider the family’s values and preferences and make treatment decisions using the best available evidence. A study published in this issue of JAMA, the Pediatric Adenotonsillectomy Trial for Snoring (PATS), provides evidence-based data on the benefits and limitations of surgical intervention in children with snoring or mild obstructive sleep apnea (OSA). 2The study supports current practice and provides further evidence to discuss surgery as part of shared decision making.
Final message In children with mild sleep-disordered breathing (SDB), adenotonsillectomy, compared with watchful waiting, did not significantly improve executive function or attention at 12 months. However, children with adenotonsillectomy had better secondary outcomes, including behavior, symptoms and quality of life, and a decrease in blood pressure and AHI, at a 12-month follow-up. |
















