Coronary heart disease (CHD) is a leading cause of mortality worldwide, with nearly 9.14 million deaths attributed to CHD in 2019. Patients with established CHD are considered to have a two- to five-fold increased risk of death or non-fatal cardiovascular events, including heart failure (HF) and stroke, resulting in a substantial number of hospitalizations, high medical care, deterioration in quality of life and disability. Therefore, it is imperative to identify modifiable risk factors to prevent recurrent cardiovascular events and premature death among patients with coronary heart disease.
Emerging evidence has suggested that unhealthy sleep behaviors are important risk factors for cardiovascular events. For example, short or long sleep duration, late chronotype, insomnia, or excessive daytime sleepiness were associated with an increased risk of cardiovascular disease (CVD). Furthermore, these sleep behaviors are often interconnected with each other in a compensatory way.
For example, insomnia or poor sleep with short objective sleep duration was associated with an increased risk of cardiovascular events, while daytime napping could mitigate the risk of cardiovascular events in people with short sleep duration. However, in most previous studies, sleep behaviors were assessed individually, ignoring the complex correlation between various sleep behaviors.
Recently, Fan et al. proposed a new sleep pattern that combined five sleep behaviors. Several studies found that a healthy sleep pattern was associated with reduced risks of CVD, HF, and cardiovascular mortality in the general population. However, to our knowledge, no study has examined the association between combined sleep behaviors and the risk of recurrent cardiovascular events in patients with coronary heart disease who were more prone to poor sleep quality.
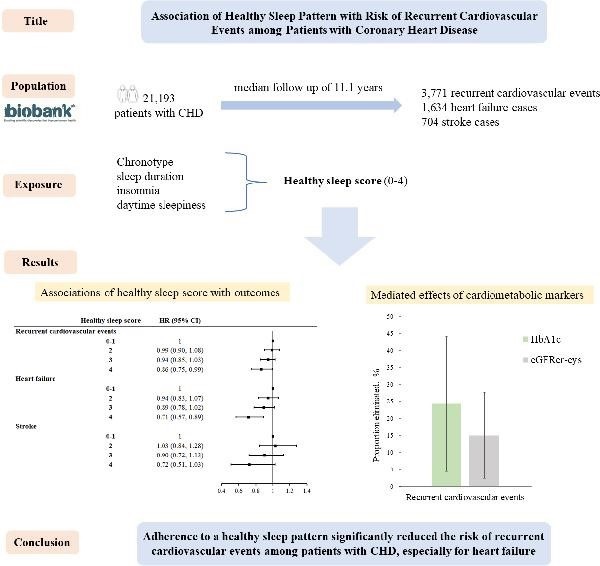
To fill the knowledge gaps, we prospectively investigated the relationship between a healthy sleep pattern and recurrent cardiovascular events in patients with coronary heart disease from the UK Biobank.
Goals
To examine the association of a healthy sleep pattern with the risk of recurrent cardiovascular events among patients with coronary heart disease (CHD).
Methods and results
This prospective cohort study included 21,193 people with coronary heart disease from the UK Biobank. A healthy sleep score was generated based on a combination of chronotype, sleep duration, insomnia, and excessive daytime sleepiness .
Cox proportional hazards regression models were applied to estimate associations between healthy sleep score and recurrent cardiovascular events. During a median of 11.1 years of follow-up, we documented 3,771 recurrent cardiovascular events, including 1,634 cases of heart failure and 704 cases of stroke.
After multivariable adjustment, including lifestyle factors, medical history, and duration of coronary heart disease, sleeping 7 to 8 h/day, never/rarely insomnia, and no frequent daytime sleepiness were significantly associated with a 12-22% lower risk of heart failure.
Furthermore, compared with participants who had a healthy sleep score of 0 to 1, the multivariable-adjusted HR (95% CI) for participants with a healthy sleep score of 4 was 0.86 (0.75, 0.99) for recurrent cardiovascular events, 0.71 (0.57, 0.89) for heart failure, and 0.72 (0.51, 1.03) for stroke.
Conclusions In a large prospective study of adults with coronary heart disease, adherence to a healthy sleep pattern was associated with a significantly lower risk of recurrent cardiovascular events, especially in the case of heart failure. Our findings suggested a potential benefit of healthy sleep behaviors in preventing recurrent cardiovascular events among patients with coronary heart disease. |
Discussion
In this large prospective cohort study of 21,193 people with prior coronary heart disease, a healthy sleep pattern was significantly associated with a 14% to 29% lower risk of recurrent cardiovascular events, including heart failure and stroke, independent of risk factors. traditional.
Furthermore, higher healthy sleep scores were associated with favorable levels of HbA1c, blood lipids, C-reactive protein, and eGFRcr-cys (creatinine-cystatin C equation, eGFRcr-cys). Furthermore, HbA1c and eGFRcr-cys explained between 15.0% and 24.3% of the association between healthy sleep score and the risk of recurrent cardiovascular events.
In accordance with European and American prevention guidelines, patients with a history of coronary heart disease were considered to be at substantially increased risk of recurrent cardiovascular events. Consistent with the findings of the STABILITY trial, where approximately 17% of total coronary events and non-fatal strokes were observed among patients with CHD, our study revealed that 17.8% of patients recur at least one event cardiovascular. Furthermore, it is noteworthy that patients with coronary heart disease frequently reported experiencing nightmares and poor sleep quality , which had been shown to exacerbate the prognosis of coronary heart disease by increasing cardiovascular disease risk factors such as hypertension. arterial. These findings underlined the crucial role of sleep behaviors in influencing the long-term prognosis of patients with coronary heart disease. These findings indicate that healthy sleep behaviors could be beneficial in preventing the recurrence of cardiovascular events.
















