Key points To what extent does COVID-19 in pregnancy alter the risks of adverse maternal and neonatal outcomes compared to pregnant women without COVID-19? Findings In this multinational cohort study of 2,130 pregnant women in 18 countries , women diagnosed with COVID-19 were at increased risk for a composite index of maternal morbidity and mortality. Newborns born to women diagnosed with COVID-19 had a significantly higher severe neonatal morbidity rate and severe perinatal morbidity and mortality rate compared to newborns born to women without a COVID-19 diagnosis. Meaning This study indicates a consistent association between pregnant people diagnosed with COVID-19 and higher rates of adverse outcomes, including maternal mortality, preeclampsia, and preterm birth compared to pregnant people without a COVID-19 diagnosis. |
A study of more than 2,000 women in 18 countries finds that COVID-19 increases the risk of maternal mortality, preeclampsia and premature birth.
Summary
Importance
Detailed information on the association of COVID-19 with outcomes in pregnant women compared to uninfected pregnant women is greatly needed.
Aim
To evaluate the risks associated with COVID-19 in pregnancy on maternal and neonatal outcomes compared to uninfected concomitant pregnant women.
Design, environment and participants
In this cohort study conducted from March to October 2020, involving 43 institutions in 18 countries, 2 consecutive, uninfected, unmatched women were simultaneously enrolled immediately after each woman was identified. infected, at any stage of pregnancy or childbirth, and at the same level of care to minimize bias. Women and newborns were followed until hospital discharge.
Exhibitions
COVID-19 in pregnancy determined by laboratory confirmation of COVID-19 and/or radiological pulmonary findings or 2 or more predefined COVID-19 symptoms.
Main results and measures
The main outcome measures were morbidity and mortality rates (maternal and severe neonatal/perinatal); The individual components of these indices were secondary outcomes. Models for these outcomes were adjusted for country, month of study entry, maternal age, and morbidity history.
Results
A total of 706 pregnant women with a diagnosis of COVID-19 and 1424 pregnant women without a diagnosis of COVID-19 were enrolled, all with very similar demographic characteristics (mean [SD] age, 30.2 [6.1] years).
Overweight at the beginning of pregnancy occurred in 323 women (48.6%) with a diagnosis of COVID-19 and in 554 women (40.2%) without it . Women diagnosed with COVID-19 had an increased risk of preeclampsia/eclampsia (relative risk [RR], 1.76; 95% CI, 1.27-2.43), serious infections (RR, 3.38; 95% CI, 1.63-7.01), intensive care unit admission (RR, 5.04; 95% CI, 3.13-8.10), maternal mortality (RR, 22.3; 95%, 2.88-172), premature birth (RR, 1.59; 95% CI, 1.30-1.94), medically indicated premature birth (RR, 1.97; 95% CI, 1.56-2.51), severe neonatal morbidity rate (RR, 2.66; 95% CI, 1.69-4.18), and severe perinatal morbidity and mortality rate (RR, 2.14; 95% CI, 1.69-4.18). of 95%, 1.66-2.75).
Fever and shortness of breath for any duration were associated with an increased risk of serious maternal complications (RR, 2.56; 95% CI, 1.92-3.40) and neonatal complications (RR, 4.97; 95% CI, 1.92-3.40). 95% CI, 2.11-11.69).
Asymptomatic women diagnosed with COVID-19 remained at increased risk only for maternal morbidity (RR, 1.24; 95% CI, 1.00-1.54) and preeclampsia (RR, 1.63; 95% CI , 1.01-2.63).
Among women who tested positive (98.1% by real-time polymerase chain reaction), 54 (13%) of their newborns tested positive.
Cesarean delivery (RR, 2.15; 95% CI, 1.18-3.91) but not breastfeeding (RR, 1.10; 95% CI, 0.66-1.85) was associated with a higher risk of neonatal test positivity.
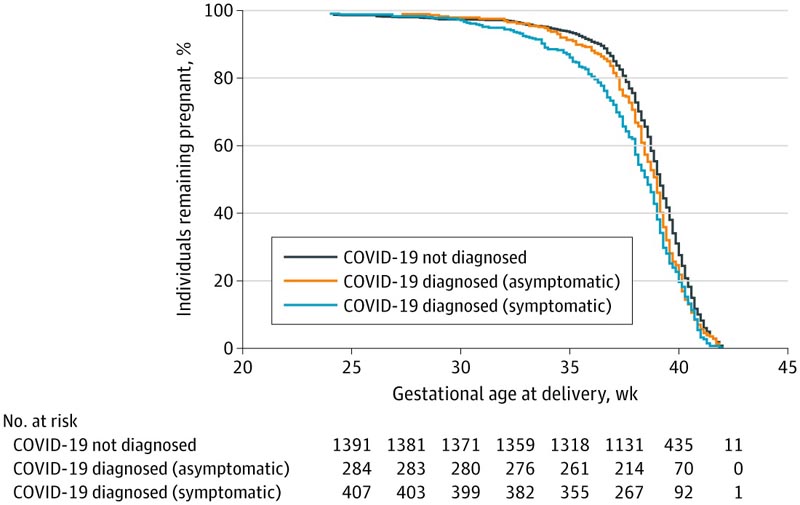
There were 1,420 women without a COVID-19 diagnosis (dark blue). In the group of women diagnosed with COVID-19, 417 women were symptomatic (light blue) and 288 women were asymptomatic (orange). There was a significant trend (P < 0.001) in shorter gestational age at delivery, moving from women without a diagnosis of COVID-19, to asymptomatic women with a diagnosis of COVID-19, to symptomatic women with a diagnosis of COVID-19 (log-rank test for trend of survivor curves). Five women with missing data were excluded from the figure.
Discussion
We conducted a large-scale prospective multinational study to evaluate symptoms and associations between COVID-19 in pregnancy and maternal and neonatal outcomes that included, to our knowledge, for the first time, immediate concomitant pregnant women without a diagnosis of COVID-19. 19 from the same populations, carefully enrolled to minimize selection bias.
We demonstrated that women with a diagnosis of COVID-19, compared to those without a diagnosis of COVID-19, had a substantially increased risk of serious pregnancy complications, such as preeclampsia/eclampsia/HELLP syndrome, ICU admission, or referral to a increased care and infections requiring antibiotics, as well as premature birth and low birth weight.
The risk of maternal mortality was 1.6%, that is, 22 times higher in the group of women diagnosed with COVID-19.
These deaths were concentrated in institutions in less developed regions, implying that when comprehensive ICU services are not fully available, COVID-19 during pregnancy can be lethal. Reassuringly, we also found that asymptomatic women with a COVID-19 diagnosis had similar outcomes to women without a COVID-19 diagnosis, except for preeclampsia.
Importantly, women diagnosed with COVID-19, who were already at high risk of preeclampsia and COVID-19 due to preexisting overweight, diabetes, hypertension, and chronic heart and respiratory diseases, 28 had almost a 4-fold increased risk of developing preeclampsia. /eclampsia, which could reflect the known association with these comorbidities and/or the acute kidney damage that may occur in patients with COVID-19.29
Our data support reports of an association between COVID-19 and higher rates of preeclampsia/eclampsia/HELLP syndrome, 19,30 but it is still unclear whether COVID-19 manifests in pregnancy with a preeclampsia-like syndrome or An infection with SARS-CoV-2 results in an increased risk of preeclampsia.
Uncertainty remains because the placentas of women with COVID-19, compared to controls, show vascular changes consistent with preeclampsia, but the state of systemic inflammation and hypercoagulability found in non-pregnant patients with severe illness and COVID-19 It is also a characteristic of preeclampsia.
It is known that in non-pregnant patients, different subtypes can predict clinical outcomes. We found that the presence of any COVID-19 symptoms was associated with increased morbidity and mortality. Specifically, rates of severe pregnancy and neonatal complications were higher in women if fever and difficulty breathing were present, reflecting systemic illness; its presence for 1 to 4 days was associated with serious maternal and neonatal complications. This observation should influence clinical care and referral strategies.
The risks of severe neonatal complications , including NICU stays of 7 days or more, as well as the Severe Neonatal Morbidity Summary Index and its individual components, were also substantially higher in the group of women diagnosed with COVID-19. . The increased neonatal risk remained after adjusting for previous preterm birth and preterm birth in the index pregnancy; therefore, COVID-19 is likely to have a direct effect on the newborn.
Overall, our results were consistent across all morbidities and primarily at RRs close to or greater than 2 for maternal and neonatal outcomes, with narrow CIs excluding unity and above 3 to 4 in several estimates. Sensitivity and stratified analyzes confirmed the observed results. They are probably conservative because overall, 41% of women diagnosed with COVID-19 were asymptomatic , a subgroup with low risk of complications. Therefore, an increased risk of morbidity and mortality should be expected for the general pregnant population, especially in low- to middle-income countries.
We found that 12.1% of newborns born to women who tested positive also tested positive, a higher figure than in a recent systematic review.
We speculate whether contamination at the time of cesarean delivery was responsible because the rate in this positive mother/newborn subgroup was 72.2%. Reassuringly, since SARS-CoV-2 has not been isolated from breast milk, breastfeeding was not associated with any increase in the rate of test-positive neonates.
Our results primarily reflect COVID-19 diagnosed in the third quarter . Therefore, women diagnosed with COVID-19 or whose pregnancy ended early are underrepresented, either because our study was exclusively hospital-based or because early infection can manifest with mild symptoms, which are ignored or treated in primary care. Alternatively, most women could have avoided the hospital until late in pregnancy or during labor. Clearly, the effect of COVID-19 in early pregnancy needs to be studied urgently.
Conclusions and relevance
|
Comments
Washington University School of Medicine/Washington University Medicine
In a global study of 2,100 pregnant women, those who contracted COVID-19 during pregnancy were 20 times more likely to die than those who did not contract the virus.
Doctors from UW Medicine and the University of Oxford led this first-of-its-kind study, published today in JAMA Pediatrics . The research involved more than 100 researchers and pregnant women from 43 maternity hospitals in 18 low-, middle-, and high-income countries; 220 of the women received care in the United States, 40 at UW Medicine. The research was carried out between April and August 2020.
The study is unique because each woman affected by COVID-19 was compared to two uninfected pregnant women who gave birth during the same period at the same hospital.
In addition to an increased risk of death, women and their newborns were also more likely to experience preterm birth, preeclampsia, and ICU admission and/or intubation.
Of the mothers who tested positive for the disease, 11.5% of their babies also tested positive, the study found.
Although other studies have looked at the effects of COVID-19 on pregnant women, this is one of the first to have a concurrent control group with which to compare the results, said Dr. Michael Gravett, one of the study’s lead authors. .
"The number one conclusion from the research is that pregnant women are not more likely to contract COVID-19, but if they do, they are more likely to become seriously ill and require ICU care, ventilation, or experience premature birth and preeclampsia." ", said. Gravett is a professor of obstetrics and gynecology at the University of Washington School of Medicine. Co-investigator Dr. Lavone Simmons is interim assistant professor of OB-GYN at the University of Washington.
One caveat, Gravett noted, was that women whose COVID-19 was asymptomatic or mild were not at increased risk for ICU care, preterm birth or preeclampsia. Approximately 40% of the women in this study were asymptomatic. Pregnant women who were obese or had hypertension or diabetes had the highest risk of severe illness, the findings showed.
Babies of women infected with COVID-19 were more likely to be born premature; but their infections were generally mild, the study found. Breastfeeding did not appear to be related to disease transmission. However, cesarean delivery may be associated with an increased risk of having an infected newborn, the study found.
Gravett suggested that these and parallel research findings forced US states to make decisions to open vaccine eligibility to pregnant women, who were initially considered a low-risk population for severe COVID-19.
"I strongly recommend that all pregnant women receive COVID-19 vaccines," based on this research, she said.
The study demonstrates the importance of collecting large-scale, multinational data quickly during a health crisis, Gravett said. The researchers were able to complete the research and report the findings in just nine months, using the already existing infrastructure of the INTERGROWTH-21st Project, which emerged in 2012 to study fetal growth and neonatal outcomes.
















