| Introduction |
The survival rate of extremely low birth weight (ELBW) infants in the United States increased from 76.5% in 2008–2012 to 78.3% in 2013–2018, (1) rates paralleling those in Japan and Sweden. (23)
ELBW infants are at increased risk of infection because the innate immune function of their skin is underdeveloped due to their lack of a competent epidermal barrier. As a result, physicians in the NICU must pay close attention to skin care practices, particularly for periviable infants.(4) However, published evidence on skin care in periviable infants (22 to 24 weeks of age) gestation) is extremely limited, in part because ELBW infants are frequently excluded from randomized controlled trials.(5)(6)
Some general preventive measures and barrier maturation techniques for ELBW infants are summarized in Table.
Skin lesions in ELBW infants include epidermal detachment, diaper rash, extravasation injury, and pressure injury.(7) Several reports of validated quality improvement methods have resulted in a decrease in skin complications in infants. with EBPN.(8)(9)
In this review, the authors describe the challenges of skin care in infants with ELBW and summarize current skin care strategies to prevent skin injury, minimize damage when it occurs, and improve innate skin immunity.
| Skin and microbiome development in ELBW infants |
> Development of the skin of the premature
The skin of premature babies has 2 different but interdependent components: the epidermis and the dermis. Skin development transitions from an embryonic phase to a fetal phase around 2 months of gestation when important morphogenetic events occur, including the formation of a 2-layer epidermis. These 2 layers are the basal layer, which gives rise to the future definitive epidermis, and the transitional layer of the periderm, which covers the fetus and provides a nutritional interface with the amniotic fluid.(10)
After birth, neonatal skin changes as it transitions from exposure to amniotic fluid to the extrauterine environment.
In ELBW babies, the skin functions as a barrier against insensible water loss, develops an acid mantle, and prevents infections. The provision of innate immunity of the skin through Langerhans cells, pro- and anti-inflammatory cytokines, structural proteins, lipids, acidic skin surface, and the stratum corneum (SC) is vital for survival in ELBW infants.(11) ) (12)
The outermost layer of the epidermis is the EC, which is structurally immature and deficient in ELBW infants. While a full-term baby has approximately 15 layers of EC, a premature baby at 28 weeks gestation has only approximately 2 to 3 layers and a periviable baby may be completely deficient in EC.(13)(14)(15)
EBPN skin is more permeable to water loss from the inside and exposure to irritants from the outside, creating risks including thermal instability, electrolyte imbalance, skin trauma/wounds (skin peeling, burns, blisters). ) and infection.(16)(17)(18) Additionally, dermal collagen deficiencies increase susceptibility to mechanical forces, such as skin tears and pressure injuries.(19)
Although barrier development and maturation occur after birth, with exposure to drier conditions, ELBW skin is not fully competent, nor is it comparable to full-term infant EC even 1 month after birth.(20) (20) 21) (22) (23)
An acidic skin mantle (pH ≈4 to 6) is necessary for the formation of an effective skin barrier, allowing precursors to form charamides to structure the EC lipid bilayer and promote desquamation.(24)(25) )(26) An acidic skin pH is also essential for bacterial homeostasis, skin colonization with commensals, and inhibition of pathogenic bacteria such as Staphylococcus aureus .(27)(28)(29)
The alkaline pH of the skin at birth decreases slowly in infants with birth weight less than 1000 g and lower gestational age compared to infants with higher birth weight and older gestational ages. (30) Although full-term babies achieve an acidic skin surface between 4 and 8 weeks after birth, ELBW infants require a longer period.(30)
> Skin microbiome
It is unknown whether current ELBW skin care practices affect the development of the “proper” (commensal) microbiota necessary for optimal innate immune function. Initial colonization of the skin depends on the mode of delivery: babies born by cesarean section have predominantly maternal skin commensals ( Staphylococcus , Streptococcus , Corynebacterium , etc.), while babies born vaginally are dominated by Lactobacillus species . (31) Exposure to chorioamnionitis, perinatal antibiotics, probiotics, and environmental factors likely influence the diversity of the developing microbiome (in richness and evenness).
Partly due to their immature skin barrier, ELBW babies are at risk for inflammation and infection, which is influenced by the developing microbiome.(32)(33)
The skin of premature babies has a lower bacterial diversity than the skin of full-term babies.(34)
Microbiome diversity is similar across body sites until around 4 to 8 weeks of age, after which site-specific maturation occurs. Staphylococcus , Cornebacterium and Prevotella relative to Brevundimonas , Flavobacterium and Sphingobacterium are more abundant in premature babies and the Shannon diversity index (a measure of species diversity) is lower.(34)
In ELBW infants, the amount of Staphylococcus is 4 times greater on the skin in front of the intestines and 2 times greater in the skin in front of the oral cavity.(35) The maternal and skin microbiomes of full-term newborns are similar at 6 weeks postnatal age.(31)
| Skin Care Challenges in ELBW Babies |
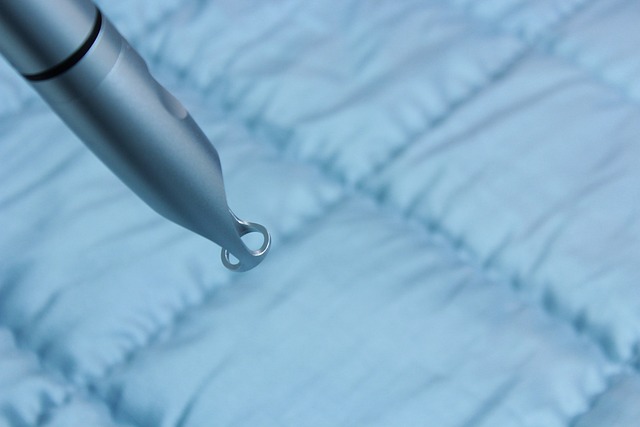
The immature skin of ELBW is susceptible to friction injuries not only during invasive life-sustaining interventions (e.g., central line insertion, intubation) but also during routine care interventions. Epidermal detachment (caused by adhesives, rubbing, friction, removal of monitor cables), skin tears, excoriation, abrasions, cuts, burns (from antiseptics), blisters and pressure injuries are observed in at least 80% of babies born between 21 and 24 weeks of gestation.(36)
Placing babies with ELBW in high humidity environments makes the skin surface very moist, delays maturation/cornification of the skin barrier, and creates conditions for bacterial growth.
Skin permeability (e.g., to topical agents) is greater at high relative humidity (RH) (> 90%) than at low RH.(37) High RH is at odds with decreasing RH, which is necessary for optimal maturation/cornification of the skin. A decrease in RH (e.g., from 80% to 85% to 50%) is necessary for skin maturation/cornification.(22)(38) (39)(40)(41)
Infants born at 23 to 25 weeks’ gestation who were maintained at 85% RH for 7 days followed by 75% or 50% RH for 4 weeks demonstrated improved skin barrier integrity if the maintenance RH was 50%.(22) NICUs where ELBW babies are covered with plastic wrap and placed under radiant heat create an environment of 50% RH that promotes maturation of the skin barrier(4)( 42)(43); however, this approach is challenged by frequent fluid and electrolyte imbalances.
Several different dressing products can be used for ELBW babies. Although the treatment of skin lesions requires dressings that optimize hydration to facilitate wound healing (as described below), different types of dressings are used to control moisture and prevent skin lesions.
Applying soft, low-adherence, water-absorbent, non-damaging silicone dressings to the skin surface of infants with ELBW can manipulate “local” skin surface moisture. These dressings "remove" moisture, dry the skin surface and create serum stress that facilitates barrier maturation. Qualitatively, soft silicone foam dressings have been shown to reduce skin surface moisture in ELBW infants.(44)(45) These dressings significantly reduce the moisture that accumulates in the skin under continuous positive pressure masks in the respiratory tract.(46)
Water vapor permeable (semipermeable) dressings facilitate the development of the skin barrier when left in place long enough so that epidermal detachment does not occur upon removal.(47)(48)(49) However, even with short periods use, transparent waterproof dressings (e.g., Tegaderm™) have caused injury (epidermal detachment) in extremely preterm infants.
Similar strategies were applied to high-exuding wounds using super-absorbent dressings to substantially reduce maceration of the surrounding skin.(50) Placing a moisture-wicking cloth containing silver in the folds of the neck and around the tubes and Gastric drains have been shown to absorb moisture and prevent skin compromise in pediatric patients 3 months to 2 years of age.(51) However, products containing silver are not recommended for babies with ELBW due to their possible toxicity.
Another challenge with skin care for ELBW babies is dirt removal and bathing.
Infants exposed to specific infections (e.g., human immunodeficiency virus, hepatitis, herpes) are rinsed with a solution of warm water and an approved cleanser to rapidly remove colonized infectious agents after birth, as tolerated.( 52) Routine full-body bathing should be delayed in ELBW infants until at least 2 weeks postpartum and the frequency of bathing may be limited to every 3 to 4 days, as tolerated.(53)
Normal saline at body temperature is recommended to initially cleanse the baby’s skin.(7)(54)(55)(56)(57)(58)(59)(60) Cleansing agents (soaps/shampoos) can be used after 28 weeks postmenstrual age (minimum).
When used, these products should not contain known irritants (e.g., sodium lauryl sulfate, sodium laurel sulfate, soaps including sodium tallow, sodium cocoate, sodium stearate, sodium caprylate, sodium oleate, sodium palmitate , sodium linoleate), sensitizing (allergy-producing) ingredients (e.g., cocamidopropyl betaine, coco-betaine, coco-glucoside, decyl glucoside, caprylyl/capryl glucoside, lauryl glucoside), or fragrance.(61)
Diaper areas are particularly sensitive to skin involvement in ELBW infants.
| Skin lesions in babies with ELBW: Physiology and treatment |
Wounds heal differently in babies and adults.(62)
Infant skin can generate elastin, collagen, and fibroblasts more rapidly than that of adults.(58) Granulation tissue and extracellular matrix (ECM) develop more rapidly in infants to facilitate wound closure.(62) (63)
Despite these differences, wound healing undergoes similar stages, regardless of gestational age.
Wound healing occurs in 4 stages: 1) hemostasis, 2) inflammation, 3) proliferation and 4) remodeling/modulation.(54)(64)(65)(66)
After injury, hemostasis occurs when blood vessels undergo vasoconstriction and platelets interact with ECM components, including fibronectin and collagen, to adhere to the vessel wall.(67) Fibrinectin, fibrin, Undine thrombus and vitronectin form a clot to prevent bleeding.
Endothelial and smooth muscle cells work to restore damaged blood vessels. In the inflammatory stage, damaged tissues send a signal to immune cells (e.g., macrophages, T cells, Langerhans cells, and mast cells) to activate inflammation(68) and increase the production of cytokines and chemokines. These mediators attract neutrophils, leukocytes and monocytes to the wound and generate toxins to destroy infectious agents, produce cytokines (interleukin 1, interleukin 6, tumor necrosis factor α) and chemokines and debride necrotic tissue.(69)
Finally, macrophages engulf the bacteria and eliminate the neutrophils, signaling the completion of the inflammatory phase.
In the proliferative stage, keratinocytes, fibroblasts, macrophages, and endothelial cells interact in an orchestrated process in which keratinocytes generate metalloproteinases and produce ECM proteins to form a new basement membrane.(67) Keratinocytes move from opposite sides of the wound. where they coalesce and form new epidermal layers from the bottom to the top of the wound.
Stem cells from skin elements (e.g., hair follicles, sebaceous glands) respond to injury and contribute to the repair process.(69) Growth factors (e.g., transforming growth factor β) activate fibroblasts to produce collagen and ECM necessary for dermal repair.(67) Finally, tissue remodeling occurs through changes in the ECM and fibroblasts. The clot that formed to stop bleeding is “replaced” with fibronectin, proteoglycans and hyaluronan to create complex collagen fibrils.(70)
Skin wounds are classified according to their depth as 1) superficial, 2) partial thickness and 3) full thickness.
Superficial wounds have damage to the epidermis. They can vary in severity, ranging from loss of part or all of the SC to complete loss that also involves the basal layer. Partial thickness wounds include the epidermis and part or all of the dermis.
Full-thickness lesions extend into the subcutaneous tissue and may include fascia and muscle, particularly in ELBW infants in whom subcutaneous tissue is absent.
Two strategies are recommended for the treatment of skin wounds in infants with ELBW, namely, wet care and dry care. Reports in the literature recognize the difficulty of determining the “optimal” moisture/dryness that should be achieved for wound healing. (71)
In general, it is necessary to provide moisture to the wound, as moisture allows cell migration, cell signaling, re-epithelialization and robust ECM formation, to increase the healing rate and reduce scar formation.(72)(73)( 74)
Unaffected skin surrounding a wound may be damaged (i.e., macerated)(75)(76)(77) if wound treatment inadvertently increases moisture in those areas. Dressings play an important role in moisture management(78) to create “optimal” humidity (i.e., not too wet and not too dry). Experts recommend moderation in wound treatment in ELBW, including dry treatment.(60)
The addition of moisture can cause maceration and a delay in barrier formation in a humid incubator environment.
Dry, scaly skin is commonly seen in newborns after the transition from moist to relatively dry conditions at birth before increasing during weeks 2 to 4.(79)
The decrease in hydration and the appearance of scales is somewhat delayed in premature babies. As the premature baby’s skin barrier matures rapidly, epidermal proteins inhibit enzymes that cause the outer layers to shed.(80) Reduced shedding is protective for premature babies as maintenance of that layer helps reduce the loss of water.
The specific properties of wound dressings, including their relative occlusivity, measured as the rate of water vapor transport (moisture weight per time), and the ability to absorb liquid should be carefully considered during the care of injured skin. ELBW infants. Tuca et al demonstrated that “occlusive” dressings (i.e., those with relatively low water vapor transport rates) facilitated granulation tissue formation and are necessary for partial healing and full-thickness wounds. (66)
Completely occlusive dressings caused maceration and barrier damage due to water accumulation on the skin surface.(81) In contrast, dressings that were nonocclusive (i.e., semipermeable with relatively high water vapor transport ) promoted the re-epithelialization necessary for superficial wounds and for the last stages of partial and full thickness wounds. Unfortunately, technical properties, such as water vapor transport rates, have been reported for only a few commercially available dressings.(82)
| Conclusion |
In this review, the authors summarized the challenges of skin care in ELBW infants. They described prophylactic strategies to prevent skin injury and practical methods to promote repair and healing based on a comprehensive review of the published literature and their own documented clinical experience.
By paying careful attention to skin care and repair of skin lesions in ELBW infants, skin-related morbidities may be reduced and overall outcomes are likely to improve. However, until skin lesions are completely eradicated in ELBW infants, there is a need for continued clinical research to determine best practices with a focus on developing products designed specifically for this population.
Table : General preventive measures and barrier maturation techniques in ELBW babies
| Variable | Precautionary measures |
| General | Wash hands and wear gloves for care until skin has visibly matured Document and track skin condition with serial photographs |
| Skin surface contaminants | Minimize future skin damage by removing visible blood and potentially infected body fluids and birth contaminants from the surface of the skin and behind the ears within a few hours of birth, if the baby is clinically stable. Remove contaminants during multiple cares in the first 72 hours if the baby cannot be disturbed. Remove by moistening a 100% cotton non-adherent dressing with warm sterile saline or water; Gently pat skin dry to remove dirt. Never rub the skin. |
| General skin moisture | Identify moist areas of immature skin. Use a water vapor permeable dressing with a silicone adhesive (e.g., Mepilex Lite™) to cover large areas of skin to “wick away” surface moisture to assist in keratinization/cornification and formation of barriers. (22)(38)(39)(40)(41)(47)(48)(49)(81)(83)(84)(85)(86) Replace the bandage every 8 to 12 hours to avoid having a wet bandage against the skin. Consider removing the dressing if aggressive phototherapy is required, as the dressing may reduce the effectiveness of phototherapy. |
| Skin moisture in folds | Apply an absorbent foam dressing (e.g., Mepilex Lite™) to any moist folds or intertriginous areas such as the axilla, neck, and popliteal fossa. |
| Bedding/sheets | Place baby on clean, dry, absorbent, soft bedding to prevent skin tears and friction damage. Change top layer and wet sheets daily when moving baby for a procedure (e.g., weighing) |
| knee protection | Prevent knee abrasions (due to movement) by cutting one pad of the absorbent foam dressing (Mepilex Lite™) into a "peanut shape" for each knee. Use strips of silicone tape (e.g. Mepitac™) at the top and bottom to hold and secure the bandage and allow for flexion. Check every 12 hours and replace when dirty or wet. Note: Clear waterproof dressings and extra thin dressings (e.g. Tegaderm™, DuoDerm CGF™ and DuoDerm Extra Thin™) should not be used as they are likely to cause significant epidermal peeling upon removal. |
| Face protection | Apply a thin, semipermeable dressing, such as an extra thin dressing (e.g., DuoDerm Extra Thin™), to the cheeks to protect the skin from adhesives used to secure the feeding tube or endotracheal tube. |
| Essential devices | Apply low-adhesion, water vapor-permeable dressings to the skin under essential devices (e.g., monitor cables, feeding tubes, thermal probes) to protect the skin from adhesive injury.(87)(88) (89)(90) |
| Temperature probe | Protect your skin from adhesive damage to the reflective cover of the temperature probe by: - Cut a 5 cm piece of silicone tape (e.g. Mepitac™) - In the center, cut a corresponding piece to the size of the skin temperature probe to create a hole - Place the probe and tape on the skin so that the tape does not cover the probe - Place the reflective center on the tape and probe so that the probe is against the adhesive center; This allows the probe to accurately detect skin temperature; silicone tape (e.g. Mepitac™) protects skin from reflective core adhesive (91) - Cut a 35cm reflective core in half or use a 30cm core for minimal skin contact - If the tape curls or becomes loose, use water to remove it slowly and gently. Replace the silicone tape as necessary. |
| Cables | Dry any moisture on the skin surface before placing the electrodes on the chest. Consider wiring your back if the skin there is less injured. Use the smallest cables available.(92)(93)(94) |
| Umbilical catheter placement | Use skin antiseptics with GCH or IP to clean the smallest area possible (e.g., cord, periumbilical skin) to reduce infection.(95)(96)(97)(98) Apply antiseptic to base, the proximal cord and periumbilical abdominal skin with gentle drying (do not rub) and allow to dry. Use the lowest possible level of aqueous or alcoholic HCG (0.5-2%) to minimize exposure and risk of burns(99)(100)(101)(102)(103). At higher HCG levels (1-2%), blot excess with sterile normal saline, dry(101)(106) to minimize damage (rubbing) and prolong effectiveness.(104)(105) Do not remove Wharton’s jelly and umbilical stump antiseptic. After suturing the lines to the cord, secure the lines by wrapping the remaining sutures (long suture tail) around the catheter; create a box around the catheter with clear tape to visualize the markings and add cloth tape to the periphery to minimize abrasions.(107) Avoid sticking the lines to the periumbilical skin. |
| pressure injuries | Due to medical devices, for example, CPAP masks, electrodes, ID bands, pulse oximeter probes, and endotracheal tubes: Periodically check the skin under the devices and/or rotate the device every 8 to 12 hours to minimize the effects of pressure Note that other devices (e.g., central catheters, peripheral IV connectors) can also cause injury For CPAP: - Apply a small piece of absorbent foam dressing (e.g., Mepilex Lite™) to the bridge of nose or face under contact points of the mask to reduce moisture buildup, minimize friction effects, and redistribute pressure - Change absorbent foam dressing (e.g., Mepilex Lite™ ) as needed if moist or compressed and no longer useful for reducing pressure For babies using nasal cannulas: - Make 2 holes in a piece of thick hydrocolloid dressing (e.g., DuoDerm CGF™) and place it between the nose and cannulas - Change the waterproof dressing at each evaluation to reduce moisture. Consider rotating CPAP masks of different sizes or, alternatively, rotating masks and nasal cannulas to reduce pressure injuries (varying masks is more effective than mask and cannulas); apply protective bandage (hydrocolloid or silicone sheet) to the skin under the mask.(108)(109)(110) At each assessment, assess the bridge of the nose, tip of the nose, upper lip, nostrils nose, the nasal septum and the shape of the nose in general for erythema, cleft, skin breakdown and tissue loss. |
| HCG=chlorhexidine gluconate, CPAP=continuous positive airway pressure, IV=intravenous, IP=povidone-iodine | |
| Comment |
The present study highlights that extremely low birth weight newborns are at greater risk of developing infections because the innate immune function of their skin is not developed. Furthermore, these babies lack a competent epidermal barrier. For all of the above, the team in charge of care must pay special attention to skin care practices, especially in periviable babies.
The strategies are intended primarily to prevent skin injury, minimize damage if it occurs, and strengthen innate skin immunity. Achieving optimal skin care in this population can improve the short and long-term results of other complications that may occur.