What is the risk of future type 2 diabetes (T2D) among overweight and obese adolescents as indicated by hemoglobin A 1c (HbA 1c) levels?
In this cohort study of 74,552 adolescents aged 10 to 17 years who were overweight or obese, the incidence of type 2 diabetes increased from 1 to 69 individuals per 1,000 person-years as baseline HbA 1c increased from less than 5.5%. to 6.3% to 6.4%, with the largest increase beyond HbA 1c 6.0%.
In multivariable analyses, the risk of type 2 diabetes was 9-fold, 23-fold, and 72-fold higher for baseline HbA 1c levels of 5.9% to 6.0%, 6.1% to 6.2%, and 6.3 % to 6.4%, respectively, compared to a reference level below 5.5%.
These findings suggest that surveillance for type 2 diabetes in adolescents should be tailored based on HbA 1c level, among other risk factors.
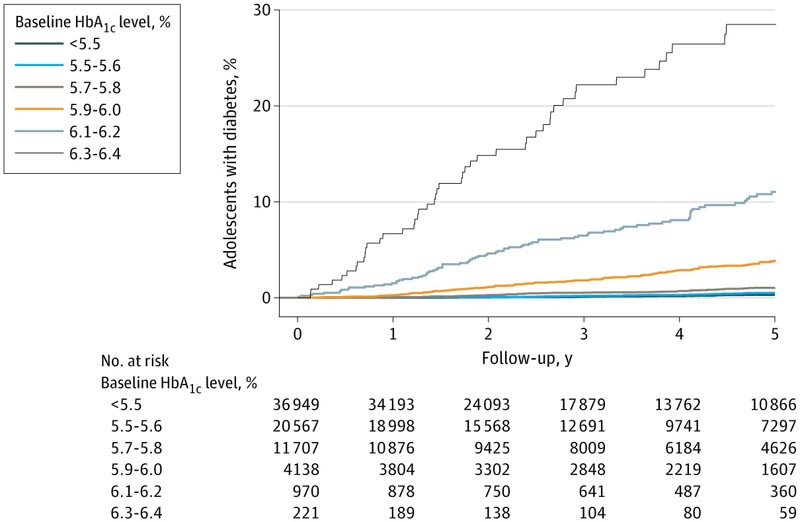
Figure : Cumulative incidence of type 2 diabetes over 5 years of follow-up by baseline hemoglobin A 1c (HbA 1c) level
HbA1c above 6% linked to much higher risk of diabetes in teens
Compared with a hemoglobin A1c (HbA1c) level of 5.5%, adolescents who were overweight or obese were 72 times more likely to have diabetes if their HbA1c was 6.3% to 6.4%.
Having a baseline hemoglobin A 1c (HbA 1c) greater than 6% has been linked to a substantially increased risk of diabetes among overweight and obese adolescents, according to research published in JAMA Network Open .
Compared with an HbA 1c level of 5.5%, overweight or obese adolescents were 72 times more likely to have type 2 diabetes (T2D) if their HbA 1c was 6.3% to 6.4%. In the same comparison, the risk of type 2 diabetes was 9-fold and 23-fold among those with HbA 1c levels of 5.9% to 6.0% and 6.1% to 6.2%, respectively. These risks varied by body mass index (BMI), age, sex, race, and ethnicity.
These findings are based on a retrospective cohort study of 74,552 adolescents with a mean (SD) age of 13.4 (2.3) years, all aged between 10 and 17 years, with a BMI equal to or greater than the 85th percentile. and without pre-existing diabetes.
Of this group, 26.9% were overweight, 42.3% moderately obese, and 30.8% severely obese. The group was predominantly Hispanic (43.6%), followed by white (21.6%), Asian or Pacific Islander (17.6%), black (11.1%), and other unknown race or ethnicity (6. 1%).
The research was conducted at Kaiser Permanente Northern California (KPNC) using electronic health record data from January 2010 to December 2019, and was supported by a grant from the KPNC Community Health program. While all of the authors have affiliations with Kaiser Permanente, they said the KPNC Community Health program had no role in designing or conducting the study.
The adolescents were followed through 2019, and during this time, 698 adolescents (0.9%) developed diabetes , 626 (89.7%) developed type 2 diabetes , and 72 (10.3%) received a diagnosis of type 2 diabetes. 1 , secondary or other type of diabetes. The overall incidence of type 2 diabetes was 2.1 (95% CI, 1.9-2.3) per 1000 person-years, and the 5-year cumulative incidence of type 2 diabetes was 1.0% ( 95% CI, 0.9%-1.1%).
The authors found that the higher the initial HbA 1c, the greater the 5-year cumulative incidence of type 2 diabetes, with the following relationships between HbA 1c and 5-year incidence:
- <5.5%: 0.3% (95% CI, 0.2%-0.4%)
- 5.5% to 5.6%: 0.5% (95% CI, 0.4%-0.7%)
- 5.7% to 5.8%: 1.1% (95% CI, 0.8%-1.3%)
- 5.9% to 6.0%: 3.8% (3.2%-4.7%)
- 6.1% to 6.2%; 11.0% (95% CI, 8.9%-13.7%)
- 6.3% to 6.4%: 28.5% (95% CI, 21.9%-36.5%)
Furthermore, and as expected, once the association between baseline HbA 1c and cumulative incidence was established, a higher baseline HbA 1c was associated with a higher risk of type 2 diabetes. Compared with reference HbA 1c 5.5 %, each level was related to the associated increased risk:
- 5.5% to 5.6%: HR, 1.7 (95% CI, 1.3-2.2)
- 5.7% to 5.8%: HR, 2.8 (95% CI, 2.1-3.6)
- 5.9% to 6.0%: HR, 9.3 (95% CI, 7.2-12.1)
- 6.1% to 6.2%: HR, 23.3 (95% CI, 17.4-31.3)
- 6.3% to 6.4%: HR, 71.9 (95% CI, 51.1-101.1)
Multivariable analyzes were adjusted for age, sex, race and ethnicity, BMI category, and neighborhood deprivation index quartile. Beyond baseline HbA 1c, the authors found other factors that were independently associated with the risk of type 2 diabetes. Being moderately or severely obese, being female, and being older put adolescents at greater risk for diabetes than if they were were overweight, male, or younger. Additionally, compared to white people, those of Asian or Pacific Islander race were more likely to develop diabetes. All of these findings were consistent with previous research. The authors noted that although black and Hispanic adolescents in the study had higher mean baseline HbA 1c, they did not have an increased risk of diabetes after adjusting for baseline HbA 1c level.
Currently, the American Diabetes Association recommends diabetes screening for overweight or obese adolescents who have reached puberty or are 10 years or older (whichever comes first) and who are at risk for diabetes based on several criteria. According to the study authors, diabetes surveillance among adolescents should take into account the study findings and be adapted to optimize identification among high-risk subgroups.
"Although HbA 1c was a strong predictor of type 2 diabetes, risk was also associated with obesity severity, age, female sex, and Asian/Pacific Islander race," the authors said. “Therefore, surveillance for type 2 diabetes in adolescents should be based primarily on HbA 1c, but should also consider these other risk factors when optimizing prevention strategies for those at highest risk. “Research is needed to determine which interventions (e.g., lifestyle intervention, pharmacotherapy, or other treatment) are most effective in preventing progression to type 2 diabetes among those at highest risk.”
Among ethnically diverse overweight and obese adolescents in this cohort study, the incidence of type 2 diabetes was relatively low, but increased with increasing baseline HbA 1c, particularly at HbA 1c levels greater than 6.0%. Although HbA 1c was a strong predictor of type 2 diabetes, risk was also associated with severity of obesity, age, female sex, and Asian/Pacific Islander race.
Therefore, surveillance for type 2 diabetes in adolescents should be based primarily on HbA 1c, but should also consider these other risk factors when optimizing prevention strategies for those at highest risk.
Research is needed to determine which interventions (e.g., lifestyle intervention, pharmacotherapy, or other treatment) are most effective in preventing progression to type 2 diabetes among those at highest risk.