
Background
In a previously reported randomized trial of standard and intensive systolic blood pressure control, data on some outcome events had not yet been adjudicated and post-trial follow-up data had not yet been collected.
Methods
We randomly assigned 9,361 participants who were at increased risk for cardiovascular disease but did not have diabetes or prior stroke to either an intensive treatment goal (systolic blood pressure, <120 mm Hg) or a standard treatment goal (blood pressure systolic, <140 mm Hg).
The primary outcome was a composite of myocardial infarction, other acute coronary syndromes, stroke, acute decompensated heart failure, or death from cardiovascular causes.
Additional primary outcome events that occurred through the end of the intervention period (August 20, 2015) were adjudicated after data locking for the primary analysis.
We also analyzed post-trial observational follow-up data through July 29, 2016.
Results
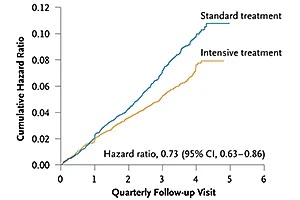 With a median of 3.33 years of follow-up, the rate of the primary outcome and all-cause mortality during the trial were significantly lower in the intensive treatment group than in the standard treatment group (rate of the primary outcome, 1. 77% per year versus 2.40% per year; hazard ratio, 0.73; 95% confidence interval [CI], 0.63 to 0.86; all-cause mortality, 1.06% per year year versus 1.41% per year; hazard ratio, 0.75; 95% CI, 0.61 to 0.92).
With a median of 3.33 years of follow-up, the rate of the primary outcome and all-cause mortality during the trial were significantly lower in the intensive treatment group than in the standard treatment group (rate of the primary outcome, 1. 77% per year versus 2.40% per year; hazard ratio, 0.73; 95% confidence interval [CI], 0.63 to 0.86; all-cause mortality, 1.06% per year year versus 1.41% per year; hazard ratio, 0.75; 95% CI, 0.61 to 0.92).
The serious adverse events of hypotension, electrolyte abnormalities, acute renal failure or failure, and syncope were significantly more common in the intensive treatment group.
When trial and post-trial follow-up data were combined (3.88 years total), similar patterns were found for treatment benefit and adverse events; however, heart failure rates no longer differed between the groups.
Conclusions Among patients who were at increased cardiovascular risk, targeting a systolic blood pressure of less than 120 mm Hg resulted in lower rates of major adverse cardiovascular events and lower all-cause mortality than targeting a systolic blood pressure of less than 140 mm Hg, both during receipt of randomized therapy and after the trial. Rates of some adverse events were higher in the intensive treatment group. |
(Funded by the National Institutes of Health; SPRINT ClinicalTrials.gov number, NCT01206062. Opens in new tab.)
















