Retinal microvascular reactivity to flickering light stimulation is a marker of endothelial function and can be quantified in vivo. Theuerle et al sought to determine whether retinal microvascular endothelial dysfunction predicts long-term major adverse cardiovascular events (MACE).
In a single-center prospective observational study, patients with coronary artery disease (CAD) or cardiovascular risk factors underwent dynamic assessment of retinal vessels in response to flashing light stimulation and were followed up. from MACE.
Retinal microvascular endothelial dysfunction was quantified by measuring peak flickering light-induced retinal arteriolar dilation (FI-RAD) and flickering light-induced retinal venular dilation (FI-RVD). In total, 252 patients underwent dynamic retinal vessel assessment and 242 (96%) had long-term follow-up.
Of the 242 patients, 88 (36%) developed MACE over a mean period of 8.6 years.
After adjustment for traditional risk factors, patients within the lowest quintile of FI-RAD had the highest risk of MACE.
Patients with lower FI-RAD were also more likely to die.
In Kaplan-Meier analysis, patients with FI-RAD responses below the cohort median of 1.4% showed reduced MACE-free survival (55.5 vs. 71.5%; log-rank P = 0.004). FI-RVD was not predictive of MACE.
This study is the first to confirm that an uncomplicated measurement of retinal arteriolar endothelial dysfunction, as measured by FI-RAD at a single time point, is a strong and independent predictor of long-term MACE in patients with CAD and risk factors. cardiovascular risk. Dynamic analysis of retinal vessels may provide additional benefit to traditional risk factors by stratifying patients at risk for cardiovascular events.
Additional clinical studies and validation of this new marker of microvascular dysfunction are required to establish the applicability of this method in the clinical field.
The endothelium forms a critical interface between circulating blood and the blood vessel wall, mediating important physiological processes including barrier function, hemostasis, inflammation, and regulation of vascular tone. Endothelial injury by proatherogenic factors results in endothelial dysfunction, an early process in the development of atherosclerosis and a contributor to its complications.
Previous work has shown that endothelial dysfunction is a systemic process that affects the coronary and cerebral circulation, in addition to smaller vessels in the periphery. Early identification of endothelial dysfunction may therefore allow risk stratification of patients with coronary artery disease (CAD).
However, current methods to clinically assess peripheral endothelial function, including digital pulse plethysmography, brachial artery flow-mediated dilation, and venous occlusion plethysmography, are cumbersome, indirect, or imprecise4-6.
The retina is unique in that it allows direct, non-invasive assessment of microcirculation in vivo.
Previous studies based on the quantitative assessment of retinal vascular caliber, measured from digital fundus photographs, show that variations in the caliber of retinal vessels are associated with diabetes and arterial hypertension and predict coronary artery disease. (CAD) and stroke independently of traditional risk factors.
The prevailing concept is that early and subtle changes in retinal vasculature may also reflect the status of cerebral and coronary circulation, providing potentially useful prognostic information for predicting CAD and major adverse cardiovascular events (MACE). However, the analysis Static analysis of retinal vessels cannot differentiate between the structural and functional characteristics of the retinal vessel wall.
Real-time quantification of changes in the caliber of retinal vessels, in response to flickering light stimulation, can be obtained by dynamic analysis of retinal vessels. Retinal vasodilation is predominantly mediated by nitric oxide release and provides a direct measurement of vascular reactivity in the retinal microcirculation.
Previous studies indicate that retinal vasodilation induced by flickering light may reflect retinal microvascular endothelial function and, consequently, may be more effective in predicting MACE than static assessment of retinal vessel caliber.
However, limited data exist regarding the ability of dynamic retinal vessel analysis to predict long-term MACE. We sought to determine whether flicker-light-induced retinal microvascular endothelial vasodilation is predictive of long-term MACE and all-cause mortality, independent of traditional factors, in patients with CAD or cardiovascular risk factors.
Graphic summary of the research
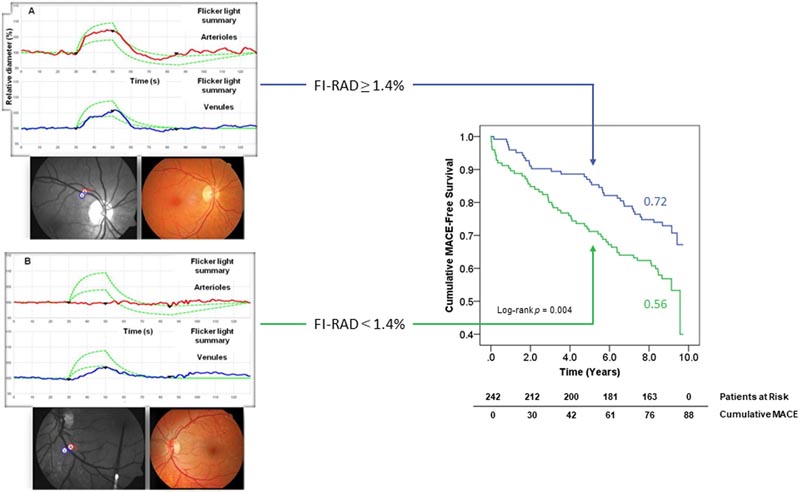
Summary Goals : Endothelial dysfunction is a precursor to the development of symptomatic atherosclerosis. Retinal microvascular reactivity to flickering light stimulation is a marker of endothelial function and can be quantified in vivo. We sought to determine whether retinal microvascular endothelial dysfunction predicts long-term major adverse cardiovascular events (MACE). Methods and results: In a single-center prospective observational study, patients with coronary artery disease (CAD) or cardiovascular risk factors underwent dynamic assessment of retinal vessels in response to flashing light stimulation and were followed up. from MACE. Retinal microvascular endothelial dysfunction was quantified by measuring peak flickering light-induced retinal arteriolar dilation (FI-RAD) and flickering light-induced retinal venular dilation (FI-RVD). In total, 252 patients underwent dynamic retinal vessel assessment and 242 (96%) had long-term follow-up. Of the 242 patients, 88 (36%) developed MACE over a median period of 8.6 years (interquartile range 6.0-9.1). After adjustment for traditional risk factors, patients within the lowest quintile of FI-RAD had the highest risk of MACE [odds ratio (OR) 5.21; 95% confidence interval (CI) 1.78-15.28]. Patients with lower FI-RAD were also more likely to die (OR 2.09, 95% CI 1.00-4.40, per standard deviation decrease in FI-RAD). In Kaplan-Meier analysis, patients with FI-RAD responses below the cohort median of 1.4% showed reduced MACE-free survival (55.5 vs. 71.5%; log-rank P = 0.004). FI-RVD was not predictive of MACE. Conclusion: Retinal arteriolar endothelial dysfunction is an independent predictor of MACE in patients with CAD or cardiovascular risk factors. Dynamic analysis of retinal vessels may provide additional benefit to traditional risk factors by stratifying patients at risk for cardiovascular events. |