Highlights
|
Long-term mortality among patients with chronic ulcers
Summary
Chronic ulcers pose a significant burden on patients and society. This study evaluated long-term mortality among patients with chronic ulcers diagnosed in a dermatology clinic between 1980 and 2010.
The mortality risk and causes of death of 3,489 ulcer patients were compared with a matched reference group of 10,399 individuals, and factors associated with increased mortality risk were examined.
Long-term mortality was increased in patients with chronic ulcers (hazard ratio (HR) 1.74) and in both men and women (HR 1.99 and 1.62, respectively).
Diabetes was the most relevant underlying cause of death (HR 8.98) and, of the immediate causes of death, sepsis was strongly associated with mortality (HR 5.86).
The risk of mortality was highest among those with arterial ulcers (HR 2.85), but also increased in patients with atypical, mixed, and venous leg ulcers.
In conclusion, patients with chronic ulcers have a higher risk of mortality regardless of age, sex, and ulcer etiology.
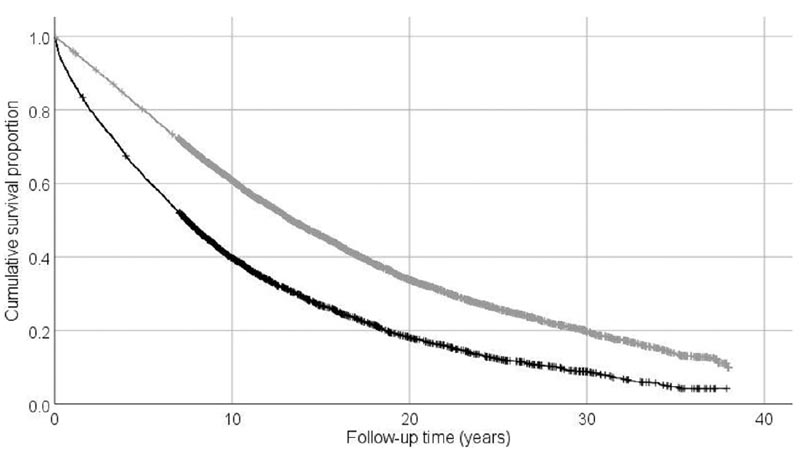
Kaplan-Meier method demonstrating the mortality of patients with chronic ulcers (black line) compared to the mortality of their reference group (gray line) during follow-up.
More information about this source textFor more information about the translation, the source text is required
Discussion
The current study established that patients with ulcers have a significantly increased risk of long-term mortality compared to their age, sex, and place of residence-matched reference group. Mortality increased in all age groups and also in both sexes, but interestingly, the HR for mortality was higher among male than female patients with ulcers and also among those who received their first ulcer diagnosis at the age of 50. years or less.
Furthermore, the risk of mortality was shown to increase regardless of the etiology of the ulcer. However, the risk was highest among patients with an arterial leg ulcer and lowest among those with a venous leg ulcer.
Similar to the findings of the current study, an association of increased risk of mortality among male patients with chronic ulcers has also been reported in other studies, and this observation has been, at least in part, explained by the overall increase of mortality associated with the male sex. However, this cannot explain the increased mortality associated with male sex in the present study, since the mortality risk of male ulcer patients was compared with that of their matched male references.
Interestingly, in the current study, men were younger than women at the time of first ulcer diagnosis and, furthermore, younger age at first ulcer was associated with a higher frequency of mortality. Therefore, age could be associated with mortality among men, or there are other explanatory factors, which we were unable to investigate in this registry-based study (e.g., comorbidities), that could explain this association.
Comorbidities are assumed to influence wound healing and, for example, the presence of diabetes has also been shown to have a notable impact on the mortality risk of patients with chronic ulcers. In addition to diabetes, common comorbidities in patients with ulcers are high blood pressure, obesity, dyslipidemia and metabolic syndrome, and a German multicenter study, consisting of 1,000 patients with ulcers, revealed that 80% of patients had one or more comorbidities relevant. Additionally, comorbidities have been shown to be more common in patients treated in wound centers, but interestingly, this does not appear to have an effect on mortality risk.
Another important finding of the current study was that the risk of mortality was elevated in all age groups, but particularly among young patients affected with a chronic ulcer, and to our knowledge, this is a finding not previously reported. Furthermore, consistent with the current results, the risk of mortality was higher for those patients with ulcers who only had one ulcer episode, although this is probably largely explained by the older age of those patients, as younger patients They have more time to develop recurrences of chronic ulcers.
In general, the knowledge that exists about the causes of death among patients with ulcers is quite limited, and studies have been directed mainly at patients with diabetic ulcers, whose main causes of death have previously been identified as cardiovascular events, diabetes and neoplasia. malignant. Therefore, the current study provided new insights into the causes of death among patients with ulcers in general and patients with different etiologies of ulcers, and the risk of mortality was highest for diabetes, and particularly increased among patients with arterial and venous leg ulcers.
It is well known that diabetes is a major risk factor for peripheral arterial disease, but diabetes has also previously been found to be common among patients with venous and vasculitic ulcers. Furthermore, mortality from ischemic heart disease was high among all, including patients with arterial and venous leg ulcers, a result consistent with a Swedish study from the 1980s.
Interestingly, mortality from digestive diseases also increased: inflammatory bowel diseases are common comorbidities of pyoderma gangraenosum, but apart from that the explanation remains obscure. Likewise, the reason for the slightly increased risk of mortality from malignancy among patients with chronic ulcers is unclear, but could be attributed to chronic inflammation associated with chronic ulcer or better diagnosis of malignancy among patients with ulcers treated in a hospital. .
Infections are a possible complication of chronic ulcers, and in this study, sepsis as an immediate cause of death was strongly associated with mortality among patients with chronic ulcers.
Furthermore, pneumonia as an underlying and also immediate cause of death increased in patients with ulcers in the current study, although to a lesser extent than sepsis, further highlighting the risk and importance of infectious complications in patients with chronic ulcers. .
In conclusion , this study demonstrated a nearly twofold increase in long-term mortality among patients with chronic ulcers. The risk of death was elevated regardless of age, sex, and ulcer etiology, but men with ulcers and those with an arterial leg ulcer were particularly at risk.
The present study highlights the importance of effective management of comorbidities, especially diabetes, as the most common morbidities associated with chronic ulcers were shown to have the highest HR of death in this study. Furthermore, timely and accurate diagnosis and treatment of infections is of utmost importance.
Although dermatologists are often key players in the diagnosis and treatment of ulcers, multidisciplinary team management is often required to optimize treatment and improve the prognosis of patients with chronic ulcers.
Meaning
|















