Key points
|
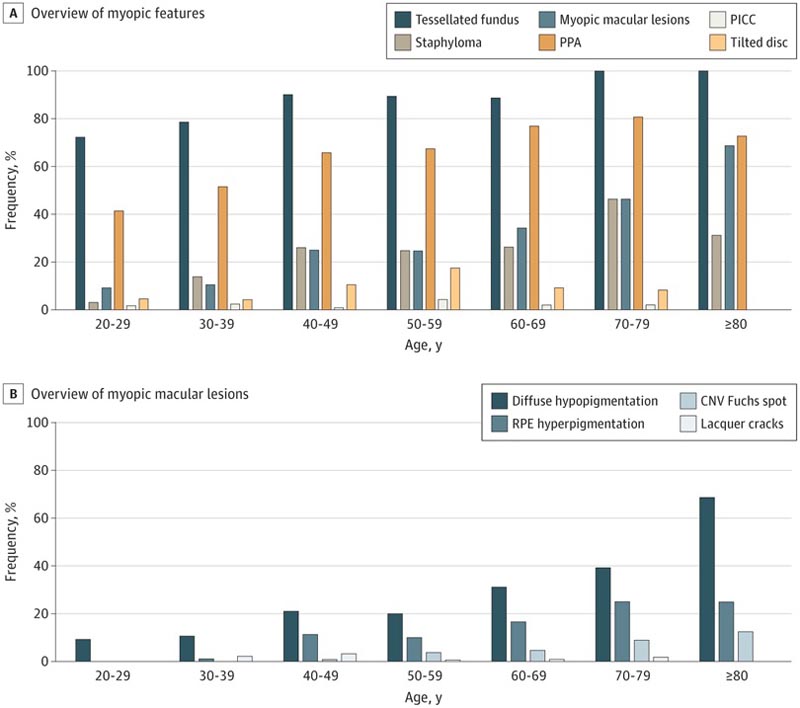
Frequency of various myopic features by age category
Comments
Among highly myopic Dutch individuals of European ancestry, myopic retinal features are common; are associated with age, spherical equivalent of refractive error (SER) and axial length (AL); and occur in all eyes with severe visual impairment, according to the results of a cross-sectional study.
The findings were published in JAMA Ophthalmology , with the authors highlighting that "the absence of treatment options for most of these retinal complications emphasizes the need for effective strategies to prevent high myopia."
Myopia is usually caused by elongation of the eye and can lead to irreversible vision loss, the researchers explained.
The presence of myopia is increasing worldwide and it is estimated that by 2050, 10% of the world’s population will be very myopic. Myopic macular degeneration (MMD) is a leading cause of visual impairment among people with myopia.
Previous research evaluating the characteristics of high myopia was primarily based on clinical data from Asian patients, while the use of the Meta-Analysis Study Group for Pathological Myopia (META-PM) international classification system among patients of European ancestry It is scarce.
To address this knowledge gap, researchers conducted a cross-sectional study to elucidate the occurrence of myopic macular features in patients with high myopia using data from the population-based Rotterdam Study (RS) and the Dutch Myopia Study (MYST). .
All individuals with a SER of -6 diopters (D) or less and an AL of 26 mm or greater included in the RS (n = 117) and MYST (n = 509) were included in the current analyses. "Both studies included extensive ophthalmologic examinations at the same research center using the same protocol," the authors wrote.
In addition to classifying retinal images from patients included in these cohorts, the researchers also conducted a systematic review to compare highly myopic people of European ancestry with those of Asian ancestry.
Of the 626 individuals of European ancestry, the mean (SD) SER was -9.9 (3.2) D and the patients had a mean age of 51.4 (15.1) years. The majority of people evaluated (61.8%) were women.
The analyzes revealed:
|
The lack of data on the prevalence of other retinal complications or features requiring high-resolution optical coherence tomography marks a limitation to the analysis, while the researchers were also unable to observe more peripheral lesions or an equatorial staphyloma. The cross-sectional design of the study prevents causal conclusions from being drawn.
Overall, the findings indicate that the prevalence of MMD is associated with AL, SER, and age among individuals of European ancestry and is not as dependent on ancestry.
"Because MMD is a major cause of VI and blindness and the (high) incidence of myopia is increasing globally, we expect the visual burden of MMD to increase accordingly," the authors concluded. "To save quality of life and productivity, future research should focus on developing innovative interventions to prevent these complications, and ophthalmic physicians should encourage myopia control."
Conclusions and relevance
In this cross-sectional study of a highly myopic Dutch population of European ancestry, myopic retinal features were common; were associated with age, SER and AL; and occurred in all eyes with severe visual impairment.
The absence of treatment options for most of these retinal complications emphasizes the need for effective strategies to prevent high myopia.















