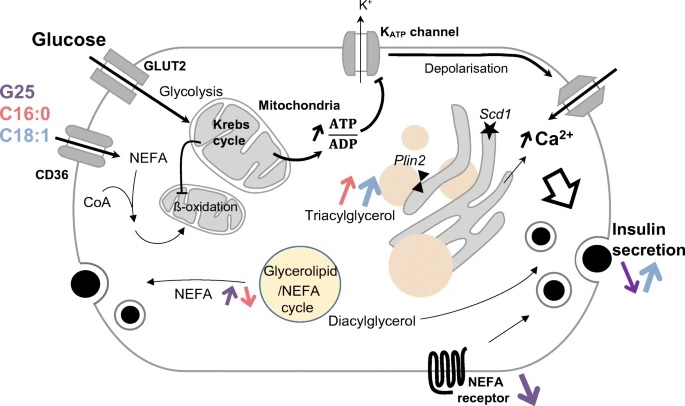
Summary Objectives/hypotheses Chronic exposure of pancreatic beta cells to elevated levels of glucose and fatty acids has been proposed to induce glucolipotoxicity . However, conflicting results suggest beta cell adaptations , which could be critical for the partial preservation of the secretory response. In this context, we delineate the expression pattern of genes related to lipid pathways along with fat storage/mobilization during glucose-stimulated insulin secretion. Methods Insulin-secreting cells were cultured for 3 days at different glucose concentrations (5.5, 11.1, 25 mmol/L) without or with 0.4 mmol/L of palmitate and oleate in complex with BSA. Transcriptomic analyzes of lipid pathways were then performed in human islets by RNA-Seq and in INS-1E cells and rat islets by quantitative RT-PCR. Fat storage was assessed in INS-1E cells by electron microscopy and Bodipy staining, which was also used to measure the rate of lipid mobilization. The secretory response was monitored during acute stimulation with 15 mmol/l glucose using an online luminescence assay for INS-1E cells and by radioimmunoassay for rat islets. Results In human islets, chronic exposure to palmitate and oleate modified the expression of a panel of genes involved in lipid management. Cultivation at 25 mmol/L glucose upregulated genes encoding glycerolipid/NEFA cycle enzymes and downregulated receptors involved in fatty acid signaling. Similar results were obtained in INS-1E cells, indicating increased capacity of the glycerolipid/NEFA cycle under glucotoxic conditions . Exposure to unsaturated C18:1 fatty acids promoted the accumulation of intracellular lipids in a glucose-dependent manner , an effect that was also observed with saturated C16:0 fatty acids when combined with the panlipase inhibitor Orlistat. After glucolipotoxic culture, intracellular fat mobilization was required for acute glucose-stimulated secretion, particularly in cells treated with oleate under glucotoxic culture conditions. The rate of lipid mobilization was determined mainly by the levels of stored fat as a direct consequence of the culture conditions rather than by energy demands, except in cells loaded with palmitate. Conclusions/interpretation Glycolipotoxic conditions promote the capacity of the glycerolipid/NEFA cycle, thus preserving part of the secretory response. The fat storage/mobilization cycle emerges as a mechanism that helps the beta cell cope with glucotoxic conditions. |
Comments
The unexpected benefits of fat in type 2 diabetes
UNIGE scientists have discovered that fat can help the pancreas adapt to excess sugar, slowing the onset of diabetes.
With almost 10% of the world’s population affected, type 2 diabetes is a major public health problem. An excessively sedentary lifestyle and a high-calorie diet favor the development of this metabolic disease by altering the functioning of pancreatic cells and making blood sugar regulation less effective.
However, fat , which is often cited as the ideal culprit, could be rehabilitated. In fact, fat does not necessarily aggravate the disease and could even play a protective role : by studying insulin-producing pancreatic beta cells, scientists at the University of Geneva (UNIGE), Switzerland, showed that these cells suffered less from excess fat. sugar when previously exposed to fat.
By investigating the cellular mechanisms at work, researchers discovered how a cycle of fat storage and mobilization allows cells to adapt to excess sugar . These results, published in the journal Diabetologia , highlight an unexpected biological mechanism that could be used as a lever to delay the onset of type 2 diabetes.
Type 2 diabetes results from a dysfunction of the pancreatic beta cells, which are responsible for insulin secretion. This affects the regulation of blood sugar levels and can lead to serious complications in the heart, eyes and kidneys.
In the 1970s fat was highlighted and the concept of lipotoxicity emerged : exposure of beta cells to fat would cause their deterioration. More recently, too much sugar has also been blamed for damaging beta cells and promoting the development of type 2 diabetes.
However, although the culpability of sugar is no longer in doubt, the role of fat in beta cell dysfunction remains ambiguous. What are the cellular mechanisms involved?
“To answer this key question, we studied how human and murine beta cells adapt to an excess of sugar and/or fat,” explains Pierre Maechler, professor at the Department of Cellular Physiology and Metabolism and the Diabetes Center of the UNIGE Faculty. of Medicine, who directed this work.
When fat lends a hand to beta cells
To differentiate the effect of fat from those of sugar, scientists exposed beta cells to excess sugar, excess fat, and then a combination of both. Sugar toxicity was confirmed for the first time: beta cells exposed to high levels of sugar secreted much less insulin than normal.
“When cells are exposed to both too much sugar and too much fat, they store fat in the form of droplets in anticipation of less prosperous times,” explains Lucie Oberhauser, researcher at the Department of Cellular Physiology and Metabolism at the UNIGE Faculty of Medicine, and first author of this work.
| “Surprisingly, we have shown that this stock of fat, instead of worsening the situation, allows insulin secretion to be restored to almost normal levels .” The adaptation of beta cells to certain fats would thus contribute to maintaining normal blood sugar levels.” |
The essential adaptive use of fat
By further analyzing the cellular changes at play, the research team realized that the fat droplets were not static reserves, but the site of a dynamic cycle of storage and mobilization.
And thanks to these released fat molecules, beta cells adapt to excess sugar and maintain almost normal insulin secretion. “This release of fat is not really a problem as long as the body uses it as a source of energy,” adds Pierre Maechler.
“To avoid developing diabetes, it is important to give this beneficial cycle the opportunity to be active, for example by maintaining regular physical activity.”
Scientists are now trying to determine the mechanism by which this released fat stimulates insulin secretion , hoping to discover a way to delay the onset of diabetes.