Background
There are complex interactions between pain and perceptions of the body part experiencing pain in musculoskeletal disorders, and the disruption of various body representations in people with chronic pain.
Introduction:
Data from multiple sources suggest that there are complex interactions between pain and perceptions of the painful body part in musculoskeletal disorders, and numerous studies have revealed alteration of various body representations in people with chronic pain. A consistent finding is that people with pain often report that the painful area feels enlarged or swollen.
Additionally, although experimental pain studies involving noxious stimulation of the skin yield mixed results, visual illusions that increase body part size have been shown to increase pain with movement in people with complex regional pain syndrome. and delayed-onset muscle soreness, suggesting a possible causal relationship between perceptions of enlargement and pain caused by movement.
Preliminary evidence indicates that disrupted body perception may be a feature of painful knee osteoarthritis (OA).
One possible reason this article is more easily supported in knee OA is that knee inflammation is relatively common in this condition. We were interested in exploring this concept, particularly the interaction between the perception of a swollen knee and objective markers of inflammation within the knee and their influence on clinical status.
The objectives of this study, therefore, were to investigate how common it is for people with knee osteoarthritis to perceive their knee to be enlarged without objective inflammation being present. Additionally, we aimed to describe the clinical characteristics of people who did and did not have perceived or objective knee swelling.
Goals:
The purpose of this study was to investigate how often people with knee osteoarthritis (OA) complain of swelling without objective evidence of swelling, and to describe the clinical characteristics of this population.
Methods:
Forty-six people with knee osteoarthritis (68.1 ± 8.8 years) participated in this cross-sectional study. Subjective and objective swelling were assessed using a knee-specific body perception questionnaire and ultrasound, respectively. Pain intensity, disability, pain-related beliefs, 2-point discrimination threshold, and quadriceps muscle strength were also assessed.
Results:
Approximately 1/3 of participants (n = 15) had subjective feelings of knee swelling in the absence of objective swelling (S only).
Fifteen participants had subjective and objective knee inflammation (S + O group) and 16 had neither subjective nor objective knee inflammation (non-S/O group).
Participants in the S only group had similar pain or disability as those in the S + O group, but had more severe pain or disability than those in the non-S/O group.
Those in the S alone group also had a larger 2-point discrimination distance threshold at the mid-knee (impaired tactile acuity) than those in the S + O group and had more dysfunctional pain catastrophizing and pain-related self-efficacy. than the other two groups.
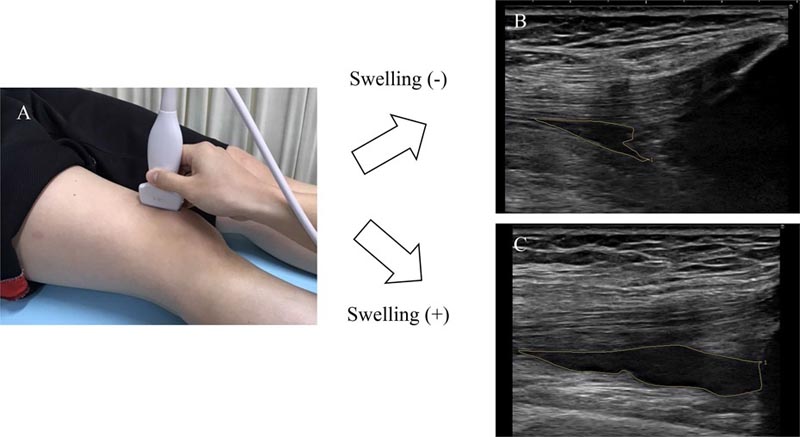
Quantitative evaluation of effusion in the suprapatellar bursa (objective swelling). (A) Ultrasound image of the suprapatellar bursa was acquired by placing a linear probe longitudinally in the suprapatellar bursa. During the examination, the transducers were placed as gently as possible, as pressure on the skin through the transducers can affect the area of the acquired effusion. Representative images of the suprapatellar swelling area: 30 mm 2 (B); 100 mm2 (C).
Discussion
This is the first study to show that about 30% of people with knee osteoarthritis report that their knee feels enlarged or swollen despite the absence of objective markers of knee inflammation.
We found that the intensity of pain and disability in those with only subjective reports of knee inflammation was similar to those who had both subjective and objective inflammation, but more severe than those without subjective or objective inflammation.
Those with only subjective reports of swelling had a larger TPD distance threshold on the medial side of the knee than those who had both subjective and objective swelling and had higher levels of pain catastrophizing and worse pain-related self-efficacy than the other two. groups.
Conclusion: Our results show that some people with knee pain experience subjective sensations of knee swelling without evidence of objective swelling detected by ultrasonography and that this group has severe pain and functional disability. Additionally, these people appear to have lower tactile acuity, lower muscle strength, and more dysfunctional beliefs about knee pain. Longitudinal data are needed to better understand how these factors interact. Specific exploration of altered knee perception could be useful in people with knee osteoarthritis and targeting any maladaptive size perception may be a potential treatment target for this group. |















