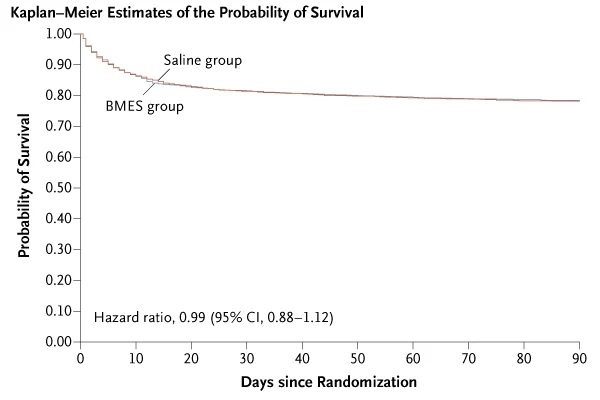
Background It is not known whether using balanced multielectrolyte solution (BMES) instead of 0.9% sodium chloride solution (saline) in critically ill patients reduces the risk of acute kidney injury or death. Methods In a double-blind, randomized controlled trial, we assigned critically ill patients to receive BMES (Plasma-Lyte 148) or saline as fluid therapy in the intensive care unit (ICU) for 90 days. The primary outcome was death from any cause within 90 days of randomization. Secondary outcomes were receipt of new renal replacement therapy and maximum increase in creatinine level during the ICU stay. Results A total of 5037 patients were recruited from 53 ICUs in Australia and New Zealand: 2515 patients were allocated to the BMES group and 2522 to the saline group. Death within 90 days of randomization occurred in 530 of 2433 patients (21.8%) in the BMES group and 530 of 2413 patients (22.0%) in the saline group, with a difference of −0.15 percentage points (95% confidence interval [CI], -3.60 to 3.30; P = 0.90). New renal replacement therapy was started in 306 of 2403 patients (12.7%) in the BMES group and in 310 of 2394 patients (12.9%) in the saline group, with a difference of −0. 20 percentage points (95% CI, −2.96 to 2.56). The mean (±SD) maximum increase in serum creatinine level was 36.6±94.0 μmol per liter (0.41±1.06 mg per deciliter) in the BMES group and 36.1±90. 2 μmol per liter (0.41±1.02 mg per deciliter) in the saline group, for a difference of 0.5 μmol per liter (95% CI, -4.7 to 5.3) (0 .01 mg per deciliter [95% CI, -0.05 to 0.06]). The number of adverse events and serious adverse events did not differ significantly between the groups.
Conclusions We found no evidence that the risk of death or acute kidney injury among critically ill adults in the ICU was lower with the use of BMES than with saline. (Funded by the National Health and Medical Research Council of Australia and the Health Research Council of New Zealand; PLUS ClinicalTrials.gov number, NCT02721654.) |
Comments
New research into intravenous fluids used in intensive care shows that the commonly used saline solution is as effective at keeping people alive and their organs functioning as more expensive balanced solutions.
The results not only give doctors greater certainty about the safety and benefits of saline , but also have broader implications for treatment availability and costs around the world.
“Almost all patients admitted to the Intensive Care Unit (ICU) will receive intravenous fluids for resuscitation or as part of standard treatment,” said Professor Simon Finfer AO, ICU doctor and senior investigator at the George Institute. .
“However, the best fluid choice has been a long-standing topic of debate, as some fluids were approved and cleared for use based on trials in a small number of patients seeking only short-term results.”
Plasma-Lyte 148® is a type of intravenous fluid that more closely matches the body’s normal levels of certain minerals, known as balanced multiple electrolyte solutions or BMES. The use of BMES has increased since concerns were raised about increased rates of kidney injury and death associated with saline, although this had not been tested in clinical trials.
To address this uncertainty and help doctors choose the best fluid for their patients, George Institute researchers designed and conducted a large clinical trial, the Plasma-Lyte 148® versUs Saline (PLUS) study, involving more than 5000 patients at 53 sites in Australia and the United States. New Zealand.
They recruited adult patients admitted to participating ICUs during the study period who required intravenous fluid resuscitation for their underlying medical condition. Patients were followed for a period of 90 days after treatment, as previous research had shown that around one in four would be at risk of dying within this time period.
The research team primarily looked at death rates in patients who were given BMES or saline while in the ICU. At 90 days after treatment, the same number of patients in the BMES and saline groups had died.
The number of days patients required mechanical ventilation, kidney dialysis, their survival time in the ICU and in the hospital, as well as major measures of healthcare costs, were similar between the groups .
“We found no evidence that the use of a balanced multielectrolyte solution in the ICU, compared to saline, reduced the risk of death or acute kidney injury in critically ill adults,” Professor Finfer said.
Every year in Australia, 160,000 people are admitted to ICU. It is one of the most expensive aspects of healthcare, with a day in the ICU costing a minimum of $4,000. With high demand for ICU beds, resources, and expertise, even a small difference in outcomes can have significant clinical and economic effects at the population level.
In the early 1990s, up to one in seven people died in ICUs in Australia and New Zealand, prompting researchers at the George Institute to begin investigating intravenous fluid resuscitation, one of the most common treatments. used in intensive care settings.
This initiated a fluid resuscitation research program conducted in ICUs that no one thought possible before, which has resulted in major changes in clinical treatment guidelines around the world, preventing harmful practices and saving many lives.
“PLUS is now the third high-impact randomized controlled trial of fluid therapy that we have conducted that has led to changes in the way critically ill patients are treated,” added Professor Finfer.
"In our first trial, we compared the commonly used saline solution with another fluid, albumin, and in the second trial, saline with hydroxyethyl starch or HES solution that was also widely used for fluid resuscitation around the world" .
"We found that saline was as good as albumin and better for patients with traumatic brain injury, and saline had similar results to HES without the associated toxicity."
“Our researchers have changed the way the medical world thinks about intravenous fluids and have shown that the choice of fluid should be treated with the same care and attention as the prescription of any medication,” added Professor Finfer.