Heterogeneity of treatment effects in an analysis of pooled individual patient data from randomized trials of device closure of patent foramen ovale after stroke
Key points Which patients with stroke associated with patent foramen ovale (PFO) could benefit from PFO closure? Findings In this meta-analysis of individual participant data that included 6 randomized clinical trials with 3740 patients with cryptogenic stroke and PFO, PFO closure plus medical treatment, compared with medical treatment alone, was associated with a variable reduction in stroke risk. recurrent stroke among subgroups with different probabilities that the stroke was causally related to the PFO. For patients classified as unlikely (i.e., with vascular risk factors and without high-risk PFO features), the hazard ratio (HR) was 1.14, but was not statistically significant; for those classified as possible or probable , the HRs were 0.38 and 0.10, respectively, both statistically significant. Meaning Applying a multivariate causal classification system to the results of randomized trials distinguished subgroups that may benefit from PFO closure from those who are unlikely to benefit. |
Importance
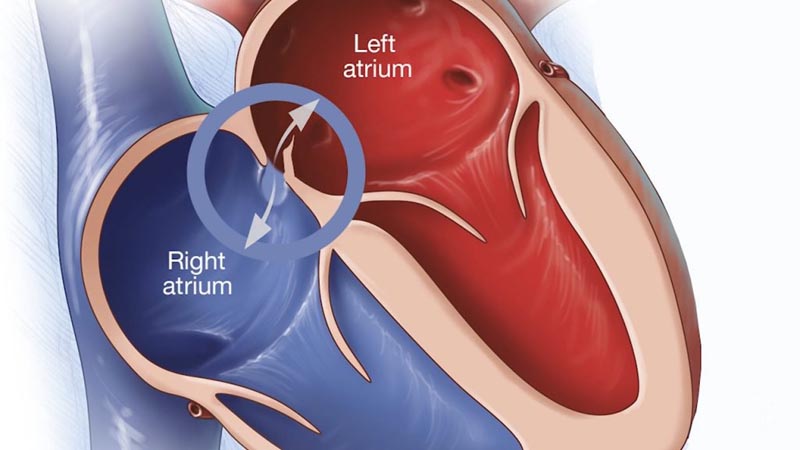
Strokes associated with patent foramen ovale (PFO) comprise approximately 10% of ischemic strokes in adults aged 18 to 60 years.
While device closure decreases the risk of stroke recurrence overall, it is often unclear what the best treatment is for any individual.
Aim
To evaluate the heterogeneity of the treatment effect of PFO closure on stroke recurrence based on previously developed scoring systems.
Design, scope and participants
Researchers from the Systematic, Collaborative, PFO Closure Evaluation (SCOPE) consortium pooled individual patient data from 6 randomized clinical trials comparing PFO closure plus medical treatment versus medical treatment alone in patients with PFO-associated stroke, including a total of 3740 participants. The trials were conducted around the world between 2000 and 2017.
Exhibitions
PFO closure plus medical treatment versus medical treatment alone. Subgroup analyzes used the Risk of Paradoxical Embolism (RoPE) score (a 10-point scoring system in which higher scores reflect younger age and the absence of vascular risk factors) and the RoPE classification system. causal probability of PFO-associated stroke (PASCAL), which combines the RoPE score with high-risk PFO features (either atrial septal aneurysm or large shunt) to classify patients into 3 causal relationship categories : unlikely, possible and probable.
Main results and measures
Ischemic stroke.
Results
During a median follow-up of 57 months (IQR, 24-64), 121 outcomes occurred in 3740 patients. The annualized incidence of stroke with medical treatment was 1.09% (95% CI, 0.88%-1.36%) and with device closure was 0.47% (95% CI, 0.88%-1.36%). 35%-0.65%) (adjusted hazard ratio [HR], 0.41 [95% CI, 0.28-0.60]).
Subgroup analyzes showed statistically significant interaction effects. Patients with low versus high RoPE score had HRs of 0.61 (95% CI, 0.37-1.00) and 0.21 (95% CI, 0.11-0.42), respectively ( P for interaction = 0.02). Patients classified as unlikely, possible, and probable using the PASCAL classification system had HRs of 1.14 (95% CI, 0.53 to 2.46), 0.38 (95% CI, 0.22 to 0. .65) and 0.10 (95% CI, 0.03 to 0.35), respectively (P for interaction = .003). The absolute risk reduction at 2 years was -0.7% (95% CI, -4.0% to 2.6%), 2.1% (95% CI, 0.6%-3 .6%) and 2.1% (95% CI, 0.9%-3.4%) in the unlikely, possible, and probable PASCAL categories , respectively.
Device- associated adverse events were generally higher among patients classified as unlikely; Absolute increases in the risk of atrial fibrillation beyond day 45 after device randomization were 4.41% (95% CI, 1.02% to 7.80%), 1.53% (95% CI, 0.33% to 2.72%) and 0.65% (95% CI, -0.41% to 1.71%) in the unlikely, possible, and probable PASCAL categories, respectively.
Conclusions and relevance
Among patients aged 18 to 60 years with PFO-associated stroke, the reduction in risk of recurrent stroke with device closure varied among groups classified by their odds that the stroke was causally related to PFO. The application of this classification system has the potential to guide individualized decision making.
Comments
Trials evaluating patent foramen ovale (PFO) closure in patients with stroke or transient ischemic attack have had mixed results. Recent studies show a modest benefit to closure.
Since the prevalence of PFO in the general population is estimated to be 20% to 25%, PFO is not considered to have a causal relationship with stroke in some patients.
It would be helpful to refine which patients are most likely to have a link between PFO and stroke. These researchers combined data from six trials that included 3740 patients (median age, 46 years; 55% men). They compared the stroke rate between patients assigned to medical treatment versus closure.
Additionally, they calculated the treatment implications of a high versus low RoPE score, which assigns points based on stroke characteristics and risk factors. Using the PASCAL classification system, which adds the size of the PFO shunt and atrial septal aneurysm to the RoPE score, they calculated treatment effects.
A large shunt was present in 45% of patients and an atrial septal aneurysm was present in 33%. The annual risk of stroke was 1.09% with medical treatment and 0.47% with PFO closure.
Treatment benefit increased with higher RoPE score (implying a higher probability that PFO was causal). In the PASCAL categories of unlikely, possible, or probable association of PFO with stroke, the hazard ratios were 1.14, 0.38, and 0.10, respectively.
The absolute risk reduction at 2 years was -0.7%, 2.1%, and 2.1% in the unlikely, possible, and probable categories. Atrial fibrillation present beyond 45 days was higher in the closure group (2.4% vs. 0.8%), as was venous thromboembolism (1.4% vs. 0.5%).
This study provides useful estimates of which patients are likely to benefit from PFO closure and which patients are unlikely to benefit.
The overall rate of recurrent stroke is low in this population, reinforcing that PFO is not a "ticking time bomb."
Shared decision making between patients, stroke specialists, and cardiologists is strongly recommended.















