Background and Objectives
Inflammatory bowel disease (IBD) is a chronic inflammatory gastrointestinal disorder with increasing global prevalence. The risk of IBD in patients with schizophrenia remains unclear. We aim to investigate the risk of new-onset IBD in patients with schizophrenia compared to matched controls.
Methods
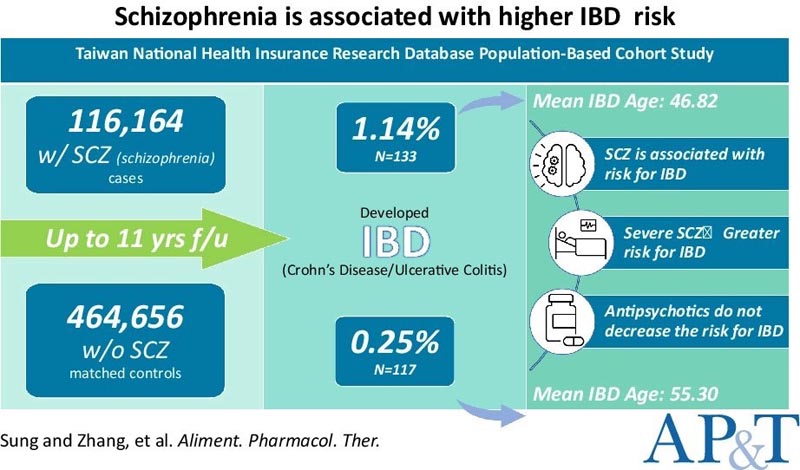
We conducted a population-based retrospective cohort study using patient data from the Taiwan National Health Insurance Research Database collected between January 1, 2001 and December 31, 2011.
Patients diagnosed with schizophrenia by board-certified psychiatrists without a prior diagnosis of IBD and matched to controls 1:4 by age, sex, residence, income level, and medical comorbidities were enrolled.
Adjusted hazard ratios (HRs) for new-onset IBD and subanalyses were determined using adjusted Cox regression analysis.
Results
Among 116,164 patients with schizophrenia and 464,656 matched controls, the overall incidence of IBD among patients was significantly higher (1.14% vs. 0.25%).
The average age of IBD diagnosis was 46.82 years among patients with schizophrenia, compared to 55.30 among controls.
The HR of developing IBD among patients was 3.28, with a 95% confidence interval (95% CI) of 2.49 to 4.33.
The risk of IBD was higher among patients with psychiatric admissions more than once a year (HR 7.99, 95% CI 5.25–12.15) compared with those hospitalized less frequently (HR 2.72, 95% CI 95% 2.03–3.66).
Conclusions
|
















