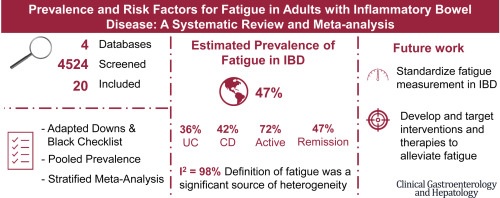
What you need to know Background Fatigue is one of the most common symptoms in inflammatory bowel disease (IBD). Unfortunately, current estimates of fatigue are limited and updated prevalence estimates are needed. Results The prevalence of fatigue in IBD is estimated at 47%. The prevalence of fatigue varied significantly by definition of fatigue and for those with active disease compared to those in remission. Implications for patient care The high prevalence of fatigue in IBD highlights the need to develop targeted therapies and standardized definitions and approaches to fatigue management. |
Inflammatory bowel diseases (IBD), including Crohn’s disease (CD) and ulcerative colitis (UC), are chronic relapsing-remitting inflammatory disorders of the gastrointestinal tract. These disorders lead to increased morbidity and substantial healthcare costs.
Fatigue is a common and disabling symptom in patients with IBD, but is poorly understood and inadequately addressed in the clinical setting.
Fatigue is described as “a persistent, overwhelming feeling of tiredness, weakness, or exhaustion that results in a decreased capacity for physical and/or mental work and is usually not relieved by adequate sleep or rest.” ”.
Fatigue in patients with IBD has a multifactorial etiology, which is not completely understood.
Fatigue affects quality of life, social functioning, and employment, and is a major concern for IBD patients.
Background and Objectives
Inflammatory bowel disease (IBD) is a chronic relapsing-remitting disease with high morbidity, substantial healthcare costs, and increasing incidence. Fatigue is one of the most common symptoms that affects quality of life and is a major concern for IBD patients.
The objective of this study was to determine the global prevalence, risk factors, and impact of fatigue in adults with IBD.
Methods
A systematic review and meta-analysis was performed. Data were retrieved from Medline, Embase, CINAHL, and PsycINFO from database inception to October 2019. A pooled prevalence of fatigue was calculated using a random effects model.
Stratified meta-analyses explored sources of heterogeneity between studies. Study quality was assessed using a checklist adapted from Downs and Black.
Results
The search yielded 4524 studies, of which 20 studies were included in the systematic review and meta-analysis. In general, the studies were of good quality. The pooled prevalence of fatigue was 47% (95% confidence interval, 41%–54%), although heterogeneity between studies was high (I2 = 98%).
The prevalence of fatigue varied significantly by fatigue definition (chronic: 28%; high: 48%; P < 0.01) and disease status (active disease: 72%; remission: 47%; P < 0.01). ,01).
Sleep disorders, anxiety, depression, and anemia were the most frequently reported fatigue-related risk factors.
Conclusions
The prevalence of fatigue in adults with IBD is high, emphasizing the importance of additional efforts to control fatigue to improve the care and quality of life of IBD patients.
Discussion
This is the largest systematic review and only meta-analysis to date providing global prevalence estimates of fatigue in IBD. Most studies were published in the last 5 years, indicating a growing interest in the study of fatigue in the context of IBD.
The overall pooled prevalence of fatigue in IBD was high (47%) with study-specific estimates ranging from 24% to 87%. In comparison, a sample of healthy individuals has been found to have a fatigue prevalence of only 5%.
However, fatigue levels in IBD resemble those of other chronic diseases, such as chronic fatigue syndrome, rheumatoid arthritis, liver disease, and irritable bowel syndrome.
A recent review of the prevalence of fatigue in more than 71,500 cancer survivors found that approximately 50% of cancer survivors reported fatigue, suggesting that patients with IBD report a similar prevalence of fatigue as cancer survivors. .
Although we expected the prevalence of fatigue to be high in IBD populations, we did not expect to find such variability in the pooled estimates. Heterogeneity between studies was partially explained by different definitions of fatigue and may also be explained by inconsistency in the use of fatigue measurement tools, in addition to possible differences in fatigue-related risk factors and their prevalence. within individual studies.
The results of this systematic review and meta-analysis demonstrated that the prevalence of fatigue in adults with IBD is high, although there is considerable heterogeneity between studies. Given the impact that fatigue has on patients living with IBD and the lack of effective therapies to manage fatigue, we recommend that future studies focus on developing a standardized definition for fatigue.
More research is also needed to better understand the impact of fatigue and fatigue-related risk factors on multiple domains of quality of life and to determine the effects of interventions to reduce fatigue burden among patients with IBD. .
Although factors contributing to fatigue and the relationship between fatigue and quality of life and fatigue-related disability have been studied in patients with IBD, none to date have evaluated all of these in the same patients, which prevents us from fully understanding these relationships.
Therefore, future studies should focus on better understanding the risk factors for fatigue and how addressing them can modify the burden of fatigue and its impact. Addressing fatigue in a clinical setting and developing interventions aimed at managing fatigue should be a high priority among patients with IBD.















