Introduction
Heart failure (HF) presents a significant social and economic burden and is increasing. The underlying pathophysiology of HF is increased intracardiac filling pressures. Identification of elevated left ventricular filling pressure (LVFP) is the cornerstone of HF diagnosis.
The gold standard methods for FPVI assessment are invasive catheterization-based methods. In routine clinical practice, right heart catheterization (RHC) is preferred for comprehensive invasive evaluation of cardiovascular hemodynamics.
In the absence of lesions in the pulmonary venules, veins, left atrium, and mitral valve, pulmonary capillary wedge pressure (PCWP), obtained by occluding the pulmonary artery, provides an accurate measurement of LVPF. Elevated PCWP is not only used to establish the diagnosis of HF4 but also identifies patients at increased risk of death, and reducing PCWP reduces HF hospitalizations.
At the population level, the invasive strategy is not feasible to diagnose and monitor treatment progress in patients with HF. Therefore, non-invasive methods are preferred and, as such, transthoracic echocardiography (TTE) is the mainstay of the initial evaluation of LVPF for phenotyping.
The main benefit of CMR is its greater precision in functional and volumetric evaluation. Currently, there is no CMR model available that predicts PFVI. It is also unclear whether such a CMR model will offer any prognostic advantage.
Therefore, we conducted this study to (i) investigate whether geometric and functional CMR parameters are associated with invasively measured PCWP in patients with suspected or proven HF; (ii) develop a CMR model to predict PCWP; and (iii) investigate whether CMR-modeled PCWP can be used for patient risk stratification.
Cardiac MRI identifies increased left ventricular filling pressure: prognostic implications
Goals
Noninvasive imaging is commonly used to estimate left ventricular (LV) filling pressure (LVFP) in heart failure (HF). Cardiovascular magnetic resonance (CMR) is emerging as an important imaging tool for subphenotyping heart failure.
However, currently, LVFP cannot be estimated from CMR. This study sought to investigate (i) whether CMR can estimate LVPF in patients with suspected HF and (ii) whether CMR-modeled LVPF has prognostic power.
Methods and results
Patients with suspected heart failure underwent right heart catheterization (RHC), CMR, and transthoracic echocardiography (TTE) (validation cohort only) within 24 hours of each other. Pulmonary capillary wedge pressure (PCWP) measured by right heart catheterization was used as a reference for LVPF.
At follow-up, death was considered the primary end point.
We enrolled 835 patients (mean age: 65 ± 13 years, 40% men).
In the derivation cohort (n = 708, 85%), two CMR metrics were associated with RHC PCWP: LV mass and left atrial volume. When applied to the validation cohort (n = 127, 15%), the correlation coefficient between RHC PCWP and CMR-modeled PCWP was 0.55 (95% confidence interval: 0.41–0.66, P < 0.0001).
Cardiovascular MRI-modeled PCWP was superior to TTE in classifying patients as having normal or elevated filling pressures (76 vs. 25%).
PCWP modeled by cardiovascular MRI was associated with an increased risk of death (hazard ratio: 1.77, P < 0.001).
In Kaplan-Meier analysis, CMR-modeled PCWP was comparable to RHC PCWP (≥15 mmHg) in predicting survival at 7 years of follow-up (35 vs. 37%, χ2 = 0.41, P = 0 ,52).
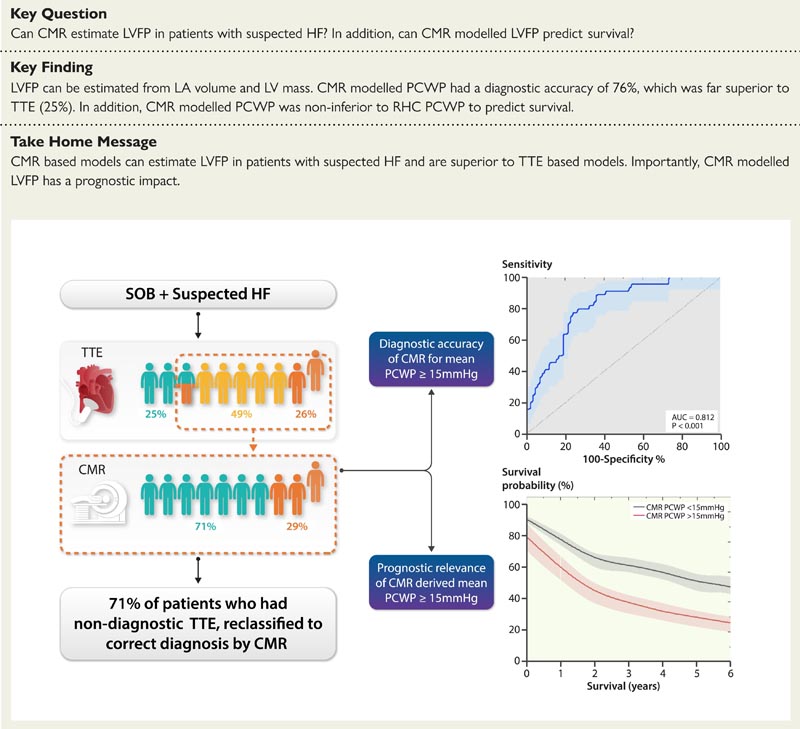
Patients presenting with dyspnea underwent TTE, CMR, and RHC. Cardiovascular MRI-modeled PCWP and TTE-estimated PCWP were compared with invasively measured PCWP. The diagnostic accuracy of our CMR model was 71% compared to 25% for TTE. In cases where TTE was nondiagnostic (indeterminate or incorrect diagnosis), CMR correctly reclassified the correct diagnosis in 71%. Furthermore, CMR-derived PCWP was an independent predictor of survival. CMR, cardiac magnetic resonance; HF, heart failure; PCWP: pulmonary capillary wedge pressure; SOB, shortness of breath; TTE, transthoracic echocardiography; RCC, right heart catheterization.
Conclusion
A physiological CMR model can estimate LVPF in patients with suspected HF. Furthermore, LVFP modeled by CMR has a prognostic role.
Discussion
The present study demonstrated that in patients with suspected heart failure, CMR volumetric variables can be used to predict elevated LVPF, significantly improving the classification provided by standard ETT assessment.
Furthermore, increased PCWP modeled by CMR was associated with increased risk of death. Notably, the prognostic power of PCWP modeled by CMR was not inferior to PCWP measured by RHC.
Any increase in intracardiac pressure due to heart failure results in remodeling of both the atrium and ventricle. In this study, we observed that invasively measured PCWP, a surrogate of LVFP, had a positive association with CMR-derived LAV and LVM.
These findings are consistent with the Frank-Starling mechanism underlying cardiovascular physiology, that is, ventricular output increases as preload (end-diastolic pressure) increases.
Comments
Using MRI scans to detect heart failure could revolutionize the way the condition is diagnosed, thanks to new research from the University of East Anglia and the University of Sheffield.
Until now, the best way to diagnose heart failure has been invasive evaluation, but it carries risks for patients. Instead, non-invasive echocardiograms, which are based on ultrasound, are often used, but they are erroneous in up to 50 percent of cases.
A new study published today shows how magnetic resonance imaging (MRI) is superior to echocardiography in diagnosing heart failure , as well as being a powerful tool in predicting patient outcomes, including death.
Lead researcher Dr Pankaj Garg, from UEA Norwich Medical School, said: “Heart failure is a terrible condition that results from increased pressure within the heart. The best method to diagnose heart failure is through invasive evaluation, which is not preferred as it carries risks.
“An echocardiogram, which is an ultrasound of the heart, is usually used to predict the pressure in the heart. However, it is not very precise. “We wanted to find out if MRIs could offer a better alternative.”
The research team studied 835 patients who received invasive assessment and MRI of the heart on the same day from the ASPIRE registry, a database of patients assessed at the Sheffield Pulmonary Vascular Disease Unit.
Dr Garg said: “We investigated whether heart MRI can predict invasively measured left ventricular filling pressure.
“Once we identified the key parameters (left atrial volume and left ventricular mass), we created an equation to non-invasively derive the pressure in the heart. This simple equation can be applied at any center in the world that performs heart MRIs. “We also tested the equation on a separate group of patients and demonstrated its reliability.”
“We showed that heart MRI is superior to echocardiography in predicting pressure inside the heart. Nearly 71 percent of patients who had incorrectly measured pressures by echocardiography had correct pressures by heart MRI.
“These findings will reduce the need for invasive evaluation. This is not only cost-effective, but also reduces risks for patients, since a heart MRI is a completely non-invasive test.”
“We also showed that heart MRI results were powerful tools for predicting whether a patient would live or die.”
“This research was not possible without the technical expertise of Norwich and Sheffield and the wealth of hemodynamic data from the ASPIRE registry,” added Dr. Garg.
The study was funded by research grants from the Wellcome Trust and the National Institute for Health and Care Research (NIHR), the research partner of the NHS, public health and social care.
Lead author Dr Andy Swift, from the University of Sheffield and consultant radiologist, said: "This simple diagnostic equation is very useful clinically and will help doctors predict pressure in the heart and diagnose heart failure."
"Testing the use of the equation in other hospitals is the next step to evaluate the benefit to patients and the reduced need for invasive testing."
"Cardiac MRI identifies elevated left ventricular filling pressure: prognostic implications" is published in the European Heart Journal on May 5, 2022.
















