Key points Ask What are the risks of neuropsychiatric disorders in adults surviving COVID-19 hospitalization and how do they compare to non-COVID severe respiratory infections? Findings In this cohort study of data from more than 8 million adults in England, during the COVID-19 pandemic, the risks of new diagnoses of anxiety disorder, dementia, psychotic disorder and bipolar disorder increased significantly in adults who survived hospitalization for COVID-19 or other severe acute respiratory infections compared to the general population. The risks of neuropsychiatric illness or initiation of related medications were similar for COVID-19 and non-COVID severe respiratory infections. Meaning The results of this study suggest that disease severity, rather than the pathogen, is a relevant factor associated with neuropsychiatric ramifications after severe respiratory infections. |
The COVID-19 pandemic has caused more than 5 million deaths worldwide and caused profound social and economic disruption. There is continued interest in various conditions and the risk of serious outcomes due to SARS-CoV-2 infection and increasing interest in its long-term effects. Although post-acute COVID-19 syndrome is not well understood, there are clinically relevant post-infection outcomes associated with several organ systems.
Pre-pandemic data suggest that people with severe acute respiratory infections (SARI) are at increased risk of subsequent neuropsychiatric illness and cognitive impairment compared to the general population.
Furthermore, previous outbreaks of the SARS virus have been associated with notable burdens of neuropsychological sequelae. Recent evidence from the US suggests that the risk of such sequelae after COVID-19 of any severity may be significantly higher than that seen after influenza or acute respiratory infections of any type, during the COVID-19 pandemic. 19.
However, such comparisons with influenza have limited follow-up, have not considered medication use, and may be problematic due to differential disease severity and atypical influenza dynamics.
A better understanding of the neuropsychiatric sequelae of severe COVID-19 and non-COVID-19 SARI is relevant to both pandemic and post-pandemic clinical practice and planning. Using electronic health record data for a population-representative cohort of over 8 million people in England, this study aims to quantify neuropsychiatric sequelae after discharge from COVID-19 hospitalization and compare findings with patients who survived hospitalization for causes unrelated to COVID-19.
Importance
People who survive severe COVID-19 may be at increased risk of neuropsychiatric sequelae. A robust assessment of these risks can help improve clinical understanding of post-COVID syndrome, aid clinical care during the ongoing pandemic, and inform post-pandemic planning.
Aim
To quantify the risks of new-onset neuropsychiatric conditions and new neuropsychiatric medication prescriptions after discharge from a COVID-19-related hospitalization, and compare them to the risks after discharge from hospitalization for other severe acute respiratory infections (SARI) during the pandemic. of COVID-19.
Design, environment and participants
In this cohort study, adults (≥18 years of age) were identified from QResearch primary care and linked electronic health record databases, including national SARS-CoV-2 testing, episode statistics hospital admissions, intensive care admissions data, and mortality records in England, from January 24, 2020 to July 7, 2021.
Exhibitions
COVID-19-related or SARI-related hospital admission (including intensive care admission).
Main results and measures
Initial diagnoses of neuropsychiatric conditions (anxiety, dementia, psychosis, depression, bipolar disorder) or first prescription of relevant medications (antidepressants, hypnotics/anxiolytics, antipsychotics) during 12 months of follow-up from hospital discharge.
Maximally adjusted hazard ratios (HRs) with 95% CIs were calculated using flexible parametric survival models.
Results
In this cohort study of data from 8.38 million adults (4.18 million women, 4.20 million men; mean [SD] age 49.18 [18.45] years); 16,679 (0.02%) survived a hospital admission for SARI and 32,525 (0.03%) survived a hospital admission for COVID-19.
Compared to the remaining population, survivors of SARI and COVID-19 hospitalization were at increased risk for subsequent neuropsychiatric diagnoses.
For example, the HR for anxiety in survivors of severe acute respiratory infections (SARI) was 1.86 (95% CI, 1.56-2.21) and for survivors of COVID-19 infection was 2.36 (95% CI, 2.03-2.74); the HR for dementia for SARI survivors was 2.55 (95% CI, 2.17-3.00) and for survivors of COVID-19 infection was 2.63 (95% CI , 2,21-3,14).
Similar findings were observed for all medications analyzed; For example, the HR for first antidepressant prescriptions in SARI survivors was 2.55 (95% CI, 2.24-2.90) and for survivors of COVID-19 infection it was 3.24 (95% CI, 2.24-2.90). 95%, 2.91-3.61).
No significant differences were observed when directly comparing the COVID-19 group with the SARI group, except for a lower risk of antipsychotic prescription in the former (HR, 0.80; 95% CI, 0.69-0.92).
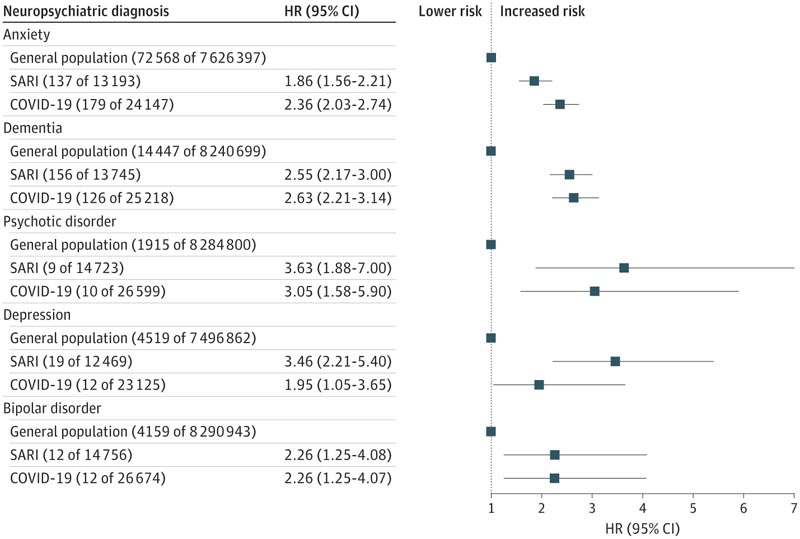
The numbers in parentheses following the general population, SARI and COVID-19 refer to the number of events and the denominator. Inclusion was determined by analysis and therefore denominator counts may vary. HR indicates hazard ratio; SARI, severe acute respiratory infections.
Conclusions and relevance In this cohort study, severe acute respiratory infections (SARI) were found to be associated with significant post-acute neuropsychiatric morbidity, for which COVID-19 is not clearly different. These results may help refine our understanding of the post-severe COVID-19 phenotype and may inform post-discharge support for patients requiring intensive care and hospital care for severe acute respiratory infections (SARI), regardless of the causative pathogen . |
Discussion
In this study, using a population-level cohort comprising linked electronic primary and secondary healthcare data sets for more than 8 million adults, we estimated that the neuropsychiatric ramifications of severe COVID-19 infection were similar to those of other SARIs. People who survived severe COVID-19 infection and other SARIs had a significantly higher risk of being diagnosed with neuropsychiatric illness and receiving antidepressant, hypnotic/anxiolytic, or antipsychotic medications in the first year after discharge compared to the population. in general.
In addition to a reduced risk of being prescribed antipsychotic medications, differences between the risks of post-COVID-19 hospitalization and post-SARI hospitalization were not significant. Although the relative risks of these outcomes in survivors of COVID-19 and SARI hospitalizations are significantly higher than for the rest of the population, the absolute risks of some formally diagnosed neuropsychiatric sequelae are low.
Post-acute outcomes associated with severe respiratory infections span physical, cognitive, and psychological domains; could be influenced by physiological disturbances, deconditioning and other stressors and are recognized under general diagnostic entities such as post-intensive syndrome, post-hospitalization syndrome and, in some cases, post-viral syndrome .
Although post-COVID-19 syndrome is of legitimate topical interest in the current context of uncertainty regarding COVID-19 survivors, our results suggest that, from the perspective of formally diagnosed or treated neuropsychiatric complications, severe COVID-19 It does not predict morbidity rates markedly different from other forms of SARI.
















