Life’s Essential 8 : Update and Improvement of the American Heart Association Cardiovascular Health Construct: A Presidential Notice of the American Heart Association.
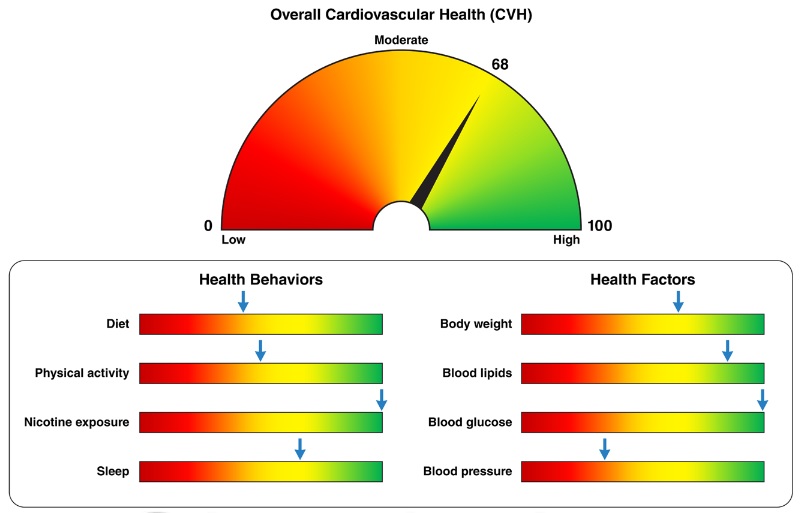
Summary In 2010, the American Heart Association defined a new cardiovascular health orientation to promote a paradigm shift from a focus solely on the treatment of disease to one that includes the promotion and preservation of positive health across the life course in populations and individuals. Extensive subsequent evidence has provided insight into the strengths and limitations of the original approach to defining and quantifying cardiovascular health. In response, the American Heart Association convened a writing group to recommend improvements and updates. The definition and quantification of each of the original metrics ( Life’s Simple 7 ) was evaluated to determine responsiveness to interindividual variation and intraindividual change. New metrics were considered and the age spectrum was expanded to include the entire life course. The fundamental contexts of social determinants of health and psychological health were addressed as crucial factors to optimize and preserve cardiovascular health. This presidential notice presents an improved approach to assessing cardiovascular health: Life’s Essential 8 . Life’s Essential 8 components include diet (updated), physical activity, nicotine exposure (updated), sleep health (new), body mass index, blood lipids (updated), blood glucose (updated), and blood pressure arterial. Each metric has a new scoring algorithm that ranges from 0 to 100 points, allowing the generation of a new cardiovascular health composite score (the unweighted average of all components) that also ranges from 0 to 100 points. Methods for implementing cardiovascular health assessment and longitudinal follow-up are discussed, as well as potential data sources and tools to promote widespread adoption in regulatory, public health, clinical, institutional, and community settings. |

Comments
Sleep duration is now considered an essential component for ideal heart and brain health. The Life’s Essential 8 ™ Cardiovascular Health Score replaces Life’s Simple 7 ™, according to a new Presidential Notice: Update and Improvement of the American Heart Association ’s Cardiovascular Health Construct , published in Circulation , the flagship peer-reviewed journal of the Asociation.
Other updates to measures of optimal cardiovascular health, now for anyone ages 2 and up, include a new guide to assessing diet; count exposure to secondhand smoke and vaping; use non-HDL cholesterol instead of total cholesterol to measure blood lipids ; and expand the measurement of blood glucose to include hemoglobin A1c , a key measure for assessing risk of type 2 diabetes.
Cardiovascular disease is the leading cause of death in the US and around the world. According to the Association’s 2022 Stroke and Heart Disease Statistics Update:
- 121.5 million people in the US have high blood pressure.
- 100 million are obese.
- More than 28 million have type 2 diabetes.
Only 1 in 4 adults reported achieving the physical activity and exercise recommended in the U.S. Department of Health and Human Services’ Physical Activity Guidelines for Americans, 2nd edition. Several research studies conducted over the past two decades indicate that more than 80% of all cardiovascular events can be prevented with a healthy lifestyle and control of known cardiovascular risk factors.
“The new sleep duration metric reflects the latest research findings: sleep affects overall health, and people who have healthier sleep patterns manage health factors such as weight, blood pressure or diabetes risk.” type 2 more effectively,” said Donald, president of the American Heart Association . M. Lloyd-Jones, MD, Sc.M., FAHA, who led the writing advisory group and is chair of the Eileen M. Foell Professor of Preventive Medicine. “In addition, advances in ways to measure sleep, such as with wearable devices, now offer people the ability to reliably and routinely monitor their sleep habits at home.”
After 12 years and more than 2,400 scientific articles on the topic, new discoveries in heart and brain health and in ways to measure cardiovascular health provided the opportunity to review each component of health in more detail. Four of the original metrics have been redefined to be consistent with the most recent clinical guidelines or to be compatible with new measurement tools. Additionally, the scoring system can now be applied to anyone over the age of 2.
Life’s Essential 8 ™ components for optimal cardiovascular health are divided into two main areas: health behaviors and health factors .
- Health behaviors include diet, physical activity, nicotine exposure, and sleep.
- Health factors are body mass index, cholesterol levels, blood sugar and blood pressure.
“The idea of optimal cardiovascular health is important because it gives people positive goals to work toward at any stage of life,” Lloyd-Jones said.
"Given the evolution of research, it was important to address some limitations of the original metrics, particularly in the ways they have been applied to people from diverse racial and ethnic populations."
Lloyd-Jones explained that some of the earlier metrics, such as diet , were not as sensitive to differences between people, nor as sensitive to changes over time within a single individual. “We felt the time was right to conduct a comprehensive review of the latest research to refine existing metrics and consider any new metrics that add value to the assessment of cardiovascular health for all people.”
Life’s Essential 8™ includes:
Diet (updated): A new guide to assessing diet quality for adults and children at the individual level (for individual health care and dietary counseling) and at the population level (for research and public health purposes).
At the population level, dietary assessment is based on daily intake of items in the Dietary Approaches to Stop Hypertension (DASH) eating pattern. The DASH-style diet score has eight components : high consumption of fruits, vegetables, nuts and legumes, whole grains, low-fat and low-sodium dairy products, red and processed meats, and sugary drinks.
For individuals, the Mediterranean Eating Pattern for Americans (MEPA) is used to assess and monitor cardiovascular health. The MEPA is a DASH-style eating pattern that can be measured with 16 yes or no questions about the weekly frequency of consumption of olive oil, vegetables, berries, meat, fish, dairy, cereals, etc. The MEPA screener does not include consumption of sugary drinks, so physicians are encouraged to ask at the time of evaluation.
Physical activity (no change): Activity is measured by the total number of minutes of moderate or vigorous physical activity per week, as defined by the US Physical Activity Guidelines for Americans, 2nd edition. The optimal level is 150 minutes or more of moderate physical activity per week or 75 minutes per week of vigorous-intensity physical activity for adults; 420 minutes or more per week for children 6 years and older; and age-specific modifications for younger children.
Nicotine Exposure (Updated): Use of inhaled nicotine delivery systems, including e-cigarettes or vaping devices, is added as the previous metric only monitored traditional combustible cigarettes. This reflects use by adults and youth and its long-term health implications. Life’s Essential 8™ also includes secondhand smoke exposure for children and adults.
Sleep duration (new): Sleep duration is associated with cardiovascular health. Measured by the average number of hours of sleep per night, the ideal level is 7 to 9 hours a day for adults. Ideal daily sleep ranges for children are 10 to 16 hours every 24 hours for children 5 years old and younger; 9 to 12 hours for ages 6 to 12; and from 8 to 10 hours for ages 13 to 18.
Body mass index (no change): The writing group recognizes that body mass index (BMI) is an imperfect metric, but it is easily calculated and widely available; Therefore, BMI remains a reasonable indicator for evaluating weight categories that can lead to health problems. BMI of 18.5 to 24.9 is associated with the highest levels of cardiovascular health. The writing group notes that BMI ranges and the subsequent health risks associated with them may differ among people of various racial or ethnic backgrounds or ancestry. This aligns with World Health Organization recommendations to adjust BMI ranges for people of Asian or Pacific Islander descent because recent evidence indicates that their risk of conditions such as CVD or type 2 diabetes is higher with a lower BMI. lower.
Blood Lipids (Updated): The metric for blood lipids (cholesterol and triglycerides) has been updated to use non-HDL cholesterol as the preferred number to monitor, rather than total cholesterol. HDL is “good” cholesterol. Other forms of cholesterol, when high, are linked to CVD risk. This change occurs because non-HDL cholesterol can be measured without prior fasting (thus increasing its availability at any time of the day and its application in more appointments) and calculated reliably among all people.
Blood Glucose (Updated): This metric is expanded to include the option of hemoglobin A1c readings or blood glucose levels for people with or without type 1 or type 2 diabetes or prediabetes. Hemoglobin A1c may better reflect long-term glycemic control.
Blood pressure (unchanged): Blood pressure criteria remain unchanged from the Association’s 2017 guidelines that established levels less than 120/80 mm Hg as optimal , and hypertension defined as systolic pressure of 130-139 mm Hg (the top number in a reading) or diastolic pressure of 80-89 mm Hg (bottom number).
The writing group also reviewed data on the impacts of stress, mental health, and social determinants of health , such as access to health care, income or education level, and structural racism, which are critical to understanding the fundamentals of health, particularly among people of diverse racial and ethnic populations.
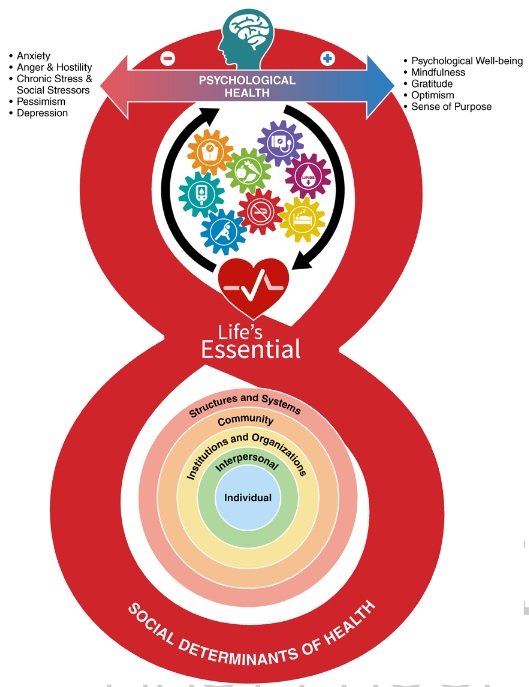
"We carefully considered the social determinants of health in our update and determined that more research is needed on these components to establish their measurement and inclusion in the future," Lloyd-Jones said. “However, social and structural determinants, as well as psychological health and well-being, are critical and fundamental factors in an individual or community’s opportunity to preserve and improve cardiovascular health. "We must consider and address all of these issues so that people have the opportunity for a full, healthy life as measured by Life’s Essential 8 ™."
Life’s Essential 8 ™ is a huge step forward in our ability to identify when cardiovascular health can be preserved and when it is not optimal. “It should boost efforts to improve cardiovascular health for all people and at all stages of life,” Lloyd-Jones concluded.
















