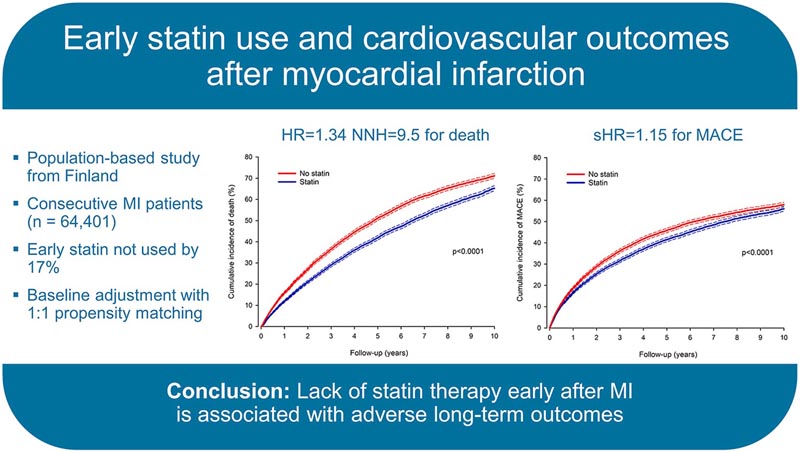
Highlights • The association of not using statins early with outcomes after myocardial infarction was studied . • 10,051 propensity-matched pairs of patients with a median follow-up of 5.9 years. • Higher all-cause mortality without early statins with NNH of 9.5 • More major adverse cardiovascular events without statins . • The results underline the importance of timely use of statins after myocardial infarction. |
Randomized trials have demonstrated the effectiveness of early treatment with 3-hydroxy-3-methyl-glutaryl-coenzyme A reductase inhibitors (statins) after myocardial infarction (MI) in reducing the risk of cardiovascular events and death. Clinical practice guidelines give statins a class IA recommendation after AMI and recommend their use in all patients regardless of low-density lipoprotein (LDL) levels. However, several patients do not use statins for secondary prevention and this is mainly due to suspected adverse events.
The key role in initiating and promoting secondary preventive treatment with statins is played by physicians who treat the patient during admission for acute myocardial infarction. However, the magnitude of harm caused by not using statins after MI in the modern era of reperfusion is not adequately known.
Placebo-controlled trials of statins, for obvious reasons, are not possible in the modern era and evidence is only available from observational data. Furthermore, long-term observational data on the impact of not using statins immediately after an AMI are limited. We set out to investigate the real-life outcome association of not using statins early after myocardial infarction in a population-based longitudinal investigation.
Background and objectives
Statin therapy is the cornerstone of secondary prevention after myocardial infarction (MI). However, many patients do not use statins . We studied the association of not using statins early after MI with adverse outcomes.
Methods
Consecutive myocardial infarction patients admitted to 20 Finnish hospitals were retrospectively studied (n = 64,401; median age 71).
17.1% did not use statins within 90 days of discharge from MI (exposure).
Differences in baseline characteristics, comorbidities, revascularization, and other evidence-based medications were balanced by propensity score, resulting in 10,051 pairs of patients with and without statinse . The median follow-up was 5.9 years .
Results
Patients who did not use statins immediately after MI had higher all-cause mortality at 1-year follow-up (15.8% vs 11.9%; HR 1.38; CI 1.30–1.46 ; p < 0.0001) and 10 years (71.1% vs 65.2%; HR 1.34; CI 1.30-1.39; p < 0.0001) in the matched cohort.
The number needed to harm for not using statins was 24.1 at 1 year and 9.5 at 10 years.
The cumulative incidence of major adverse cardiovascular events was higher at 1 and 10 years in matched patients not using statins (HRS 1.15; p < 0.0001 for both).
Cardiovascular death, new myocardial infarction, and ischemic stroke were more common without early statins.
Lack of statins was associated with outcomes regardless of sex, age, atrial fibrillation, dementia, diabetes, heart failure, revascularization, or use of other evidence-based secondary preventive medications in subgroup analyzes .
Conclusions
|
Discussion
This observational, longitudinal, population-based study investigated the association of not using statins early after myocardial infarction with outcomes. Not using statins early after myocardial infarction was independently associated with a higher rate of all-cause mortality and MACE. The NNH for omitting early statin use was 24.1 at 1 year and 9.5 at 10 years for mortality after AMI. The risk of death was higher in patients not using early statins, regardless of sex, age, major comorbidities, revascularization, or other evidence-based secondary preventive medications.
Reducing LDL cholesterol through effective lipid-lowering treatment reduces cardiovascular risk and mortality. Although other high-intensity lipid-lowering therapies are emerging, such as PCSK9 inhibitors, statins are currently the first-line medications for lipid-lowering therapy in secondary prevention. Statins act by inhibiting 3-hydroxy-3-methylglutaryl coenzyme A reductase, which is an early rate-limiting step in cholesterol biosynthesis.
Furthermore, statins may also have additional beneficial effects on plaque composition and pleiotropic effects on the endothelium, immune system, myocardium, platelets, and vascular smooth muscles that cannot be explained by cholesterol lowering. Large-scale randomized trials and observational studies have demonstrated the effect of statins in reducing the risk of major cardiovascular events. The benefits are most evident in secondary prevention after ischemic events.
However, placebo-controlled statin trials are not fully representative of the current MI population, and recent treatment modalities and observational outcome studies have focused on differences among statin users. Revascularization by percutaneous coronary intervention and the use of dual antiplatelet therapies have increased dramatically, while the prevalence of smoking, high blood pressure, and high cholesterol levels have decreased since the first statin trials.
In particular, we found that statin use starting within the first 90 days after discharge was associated with lower all-cause mortality and MACE at 1-year follow-up. This finding is consistent with previous studies showing the benefits of timely lipid reduction after myocardial infarction. However, long-term follow-up studies of non-statin users are limited. Our long-term results of early statins support previous randomized trials and underline the importance of timely statin therapy in secondary prevention after myocardial infarction.
Our study originated from the clinically simple question of what impact lack of early statin use after myocardial infarction has on long-term outcomes . Therefore, the definition of statin use was limited to the first three months after AMI, which is the maximum period in which pharmacies in Finland reimburse prescription drugs such as statins. In clinical reality, statins are already started during admission for an AMI. The concept of in-hospital initiation of higher-intensity lipid-lowering therapy (PCSK9 inhibitor) after AMI will be addressed by the ongoing EVOLVE-MI trial.
The benefits of statins far outweigh any safety concerns in secondary prevention. Suspected side effects are the leading cause of discontinuation of statin use and are likely a major determinant of patients’ hesitancy to initiate treatment in the first place. Interestingly, previous research found that 20% of statin users discontinued therapy due to suspected side effects; however, 35% restarted treatment and more than 90% tolerated restart of therapy, indicating that true statin intolerance is rare. Additionally, exaggerated claims about side effects and negative media coverage are linked to the underuse of statins.
In a randomized crossover trial, side effects were similar between statins and placebo after restarting therapy in patients who had discontinued statins due to side effects. Patients’ self-perception of cardiovascular risk after myocardial infarction is also limited, as demonstrated by a previous study that found that only 53% of young patients with myocardial infarction considered themselves at risk for heart disease. Alarmingly, an even lower proportion (46%) of patients reported that healthcare staff told them they were at risk. Although the proportion of patients using statins after myocardial infarction is increasing, there is still significant room for improvement in support for statin use after myocardial infarction.
The absolute effectiveness of statin therapy is related to overall cardiovascular risk. Paradoxically, we found that early underuse of statins is more common in patients at higher risk . Older patients, with atrial fibrillation, diabetes, heart failure, without revascularization, and without other evidence-based secondary preventive medications used statins less frequently. Additionally, statin use was less common in women after myocardial infarction. These results agree with previous observations. Notably, the risk of death after AMI was attenuated by statins regardless of age, sex, the aforementioned comorbidities, revascularization, type of AMI, or other evidence-based medications.
Statin use after myocardial infarction was associated with lower all-cause mortality in patients ≥ 80 years of age and those with dementia, in whom the evidence for statin use is more limited. Because high-risk patients are more likely to discontinue statin treatment, our results may underestimate the relative benefit of early statins in high-risk patient groups.
It is well established that high-dose statins reduce post-MI risk more than low- or moderate-dose statins, and guidelines recommend that high doses should be first-line therapy after AMI. Furthermore, statin therapy at low or moderate doses reduces long-term vascular outcomes. We found that 43% of statin users used atorvastatin or rosuvastatin shortly after myocardial infarction. In agreement, a previous Finnish study found that 33% of statin users used high-dose statins 6 months after MI, and the proportion of high doses decreased thereafter. Fortunately, however, the trend of high-dose statin use is increasing.
Adherence to statin therapy is unequivocally associated with a lower risk of death and cardiovascular outcomes. Lack of adherence to the use of statins is very common even in secondary prevention and presents an important barrier to reducing mortality and morbidity. For example, in previous studies in Germany and France, the statin discontinuation rate was around 20% during a 4- to 5-year follow-up after a recent AMI.
Final message In conclusion , approximately one- sixth of patients in this population-based study did not use statins shortly after discharge for myocardial infarction. Paradoxically, statin use was less frequent in higher-risk patients . Lack of statin treatment immediately after myocardial infarction was strongly associated with the risk of death and major cardiovascular outcomes. The risk of death was increased by not using early statins, regardless of age, sex, relevant comorbidities, revascularization, or other evidence-based secondary preventive medications. These results underscore the importance of increasing awareness of the benefits of statin use among patients and healthcare personnel to improve timely use of statins in secondary prevention after myocardial infarction. |
















