The first months after birth are a critical period for visual development. Poor visual input during this time due to a variety of structural or anatomical factors can cause severe amblyopia (decreased vision in one or both eyes due to developmental vision abnormalities in infancy or childhood). Therefore, ocular examination is an essential component of newborn screening, as early diagnosis and referral to ophthalmology can have a critical impact on the prognosis of many potentially blinding but treatable ocular conditions. (1)
| Eye anatomy and normal development |
The axial length of the eyeball undergoes rapid growth after birth, starting at approximately 16 mm and extending to 20.3 mm by 18 months of age. The size of the newborn pupil is approximately 70% of the adult pupil, and pupillary response is present at 31 weeks of gestation.
An estimated 21% of full-term newborns have physiological anisocoria (pupils of unequal size, typically < 1 mm). Pupillary asymmetry greater than 1 mm, poor response to light, or another irregular shape (eg, coloboma) warrant referral to ophthalmology. (2)
Visual development begins immediately after birth, with blinking in response to light being the earliest assessment of visual function. Fixation and more definitive visual behavior become evident around 6 to 8 weeks of age, although eye alignment can be quite variable in the first 3 to 4 months of life. Intermittent exotropia is evident in up to 70% of term neonates in the first 2 months of life and significantly decreases in incidence by 4 months; while esotropia is less common at birth, typically small-angle, and rare after 2 months of age. (2)
Nystagmus, or abnormal involuntary rhythmic eye movements with a slow movement away from the visual target followed by a second movement back to the target, can have a wide variety of causes. Infantile idiopathic nystagmus and sensory nystagmus (caused by anatomical disorders of the eye resulting in poor vision) are the most common forms seen in the neonatal period, and usually manifest a few months after birth. Therefore, poor visual behavior, persistent strabismus, or abnormal eye movements after 3 months of age warrant a thorough evaluation by an ophthalmologist.
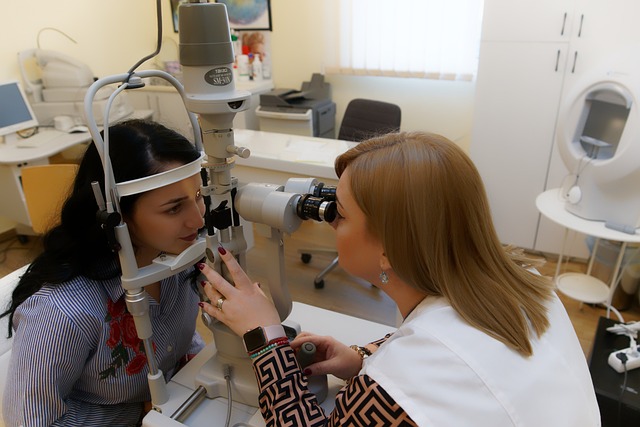
| Eye examination technique |
The newborn vision exam consists of the evaluation of the visual system through blink response to light; external examination of the orbit, eyelids and anterior segment; pupil examination; and red reflex testing to evaluate media opacities or posterior segment abnormalities.
Shining light from an ophthalmoscope directly into each eye individually should induce a blink or startle response in a newborn with normal visual function. Attention should be paid to symmetry of pupil size, even light constriction, and any abnormality in shape or appearance suggestive of an anatomical defect.
Evaluation of the anterior and external ocular structures includes inspection of the eyelids, orbits, cornea, conjunctiva, sclera, and iris. Using the direct ophthalmoscope, the red reflex is seen from the retina through the pupil. The test is performed in a dark room to facilitate maximum pupil dilation without the use of dilating eye drops.
The ophthalmoscope is held at a distance of 50 to 100 cm and both eyes are observed simultaneously to assess symmetry in color, brightness, and size of the red reflex. This is called the Bruckner Test. Each eye can then be evaluated individually for more detail. The reflection can vary from a yellow-orange to a darker red depending on the individual’s pigmentation but should be symmetrical.
A dull, absent, white (leukocoria), or asymmetric reflex or a black dot within the reflex indicates media opacity (e.g., corneal opacity, cataract), reflex block, or posterior segment abnormality (e.g., tumor). , retinal detachment) requiring referral to an ophthalmologist for a complete evaluation. (1) Possible differential diagnoses for an abnormal red reflex in the infant are described in Table 1.
| Eyelids and orbits |
> Proptosis
Proptosis, or relative anterior bulging of one or both eyes in the orbit, is rare in the neonatal period and is typically the result of an orbital mass (vascular or dermoid tumor, teratoma) or a craniofacial malformation, in which case other findings of the Clinical examination can provide clues to the diagnosis. Orbital imaging is often indicated and an ophthalmic examination is required to rule out involvement of other ocular structures (e.g., extraocular muscle restriction, globe or optic nerve compression) that can lead to vision loss if not is addressed appropriately.
> Ptosis
Congenital ptosis is most commonly the result of a developmental abnormality of the levator muscle and is typically unilateral and sporadic. Neurological causes of ptosis include congenital Horner syndrome (unilateral ptosis with heterochromia and miosis of the ipsilateral iris), cranial nerve III palsy (ptosis with "down and out" position of the eyeball), and winking syndrome Marcus Gunn mandibular syndrome (sykinnesia of cranial nerves III and V resulting in unilateral ptosis with eyelid excursion during chewing/sucking often seen during feeding). (4) An eyelid mass can cause ptosis. Severe ptosis that obstructs the visual axis is highly amblyogenic and requires urgent referral to an ophthalmologist. Non-obstructive ptosis can still cause amblyopia due to strabismus or asymmetric refractive error and therefore requires routine ophthalmic evaluation.
> Coloboma
Colobomas are full-thickness defects of the eyelid caused by failure of closure during development. They are usually sporadic and are found in the upper medial part of the eyelid; However, they are associated with 2 syndromes that should be kept in the differential when evaluating patients with eyelid defects (Goldenhar syndrome - location in the upper eyelid, Treacher Collins syndrome - location in the lower eyelid). (5) Close monitoring of the ocular surface is important because exposure can lead to corneal scarring and vision loss if untreated and is often the primary factor in deciding the timing of surgical repair.
> Abnormalities of the nasolacrimal system
A dacryocystocele is a congenital distension of the lacrimal sac that manifests at birth as a cystic subcutaneous nodule with a bluish hue located below the medial canthus. Risks of congenital dacryocystoceles include infection, with reported rates of acute dacryocystitis developing in 20% to 75% of patients, as well as respiratory compromise and difficulty feeding caused by intranasal extension of the cyst and obligatory nasal breathing of the newly born. (6)(7) Therefore, in addition to systemic antibiotics for infected dacryocystoceles, this condition also requires urgent referral for decompression and probing of the nasolacrimal system.
In contrast to dacryocystocele, typical nasolacrimal duct obstruction (NACO) presents 1 to 2 weeks after birth with persistent lacrimation and intermittent mucoid discharge from 1 or both eyes without associated palpable nodules and low risk of infection.
Initial management of an OCLN consists of observation and massage of the lacrimal sac; 80% or more cases of congenital OCLN resolve spontaneously within 12 months. (8) If not resolved by then, referral to ophthalmology for surgical probing of the nasolacrimal system to relieve obstruction is indicated. When making this diagnosis, doctors should be careful to rule out more serious causes of persistent tearing, such as congenital glaucoma, infection, or corneal injury/foreign body.
| Previous segment |
> Infection
Neonatal conjunctivitis occurs within the first 30 days after birth by definition and is an increasingly rare but serious complication in the neonatal period. All clinicians must be able to diagnose and initiate treatment of neonatal conjunctivitis promptly to minimize the risk of permanent vision loss or progression of systemic disease. Clues to diagnosis include time of onset, occurrence and amount of discharge, and associated maternal or neonatal disease.
1. Chemical conjunctivitis presents within the first 24 hours after birth with bilateral conjunctival injection and watery discharge and resolves spontaneously within 2 to 4 days. Largely attributed to the application of silver nitrate previously used as prophylaxis against bacterial conjunctivitis, chemical conjunctivitis is exceedingly rare in developed industrialized countries after switching to erythromycin ointment or 2.5% povidone-iodine solution (not currently approved for use in the United States).
2. Neisseria gonorrhea conjunctivitis presents with conjunctival injection, chemosis, significant mucopurulent discharge, and eyelid edema 3 to 5 days after birth. Rapid progression to corneal involvement leading to ulceration and perforation is the most feared complication, requiring prompt diagnosis and treatment with sterile saline irrigation to remove secretion and membranes, topical erythromycin ointment, and intravenous or intramuscular ceftriaxone. Hospitalization is usually required to monitor disseminated N. gonorrhea infection as systemic complications include arthritis, meningitis, and septicemia. These babies and their mothers should also be treated for Chlamydia at the same time.
3. Chlamydial conjunctivitis occurs 5 to 14 days after birth with conjunctival hyperemia and poor mucoid secretion, with more severe cases developing chemosis, eyelid edema, and pseudomembrane formation. Since pneumonia develops in up to 20% of these children, hospitalization may be necessary. Treatment consists of oral erythromycin and topical erythromycin ointment.
4. Herpes simplex virus keratoconjunctivitis occurs in children 1 to 2 weeks of age with periocular vesicular skin lesions, eyelid edema, conjunctival injection, and nonpurulent discharge. Corneal involvement includes microdendrites and geographic ulcers that can be identified with fluorescein staining and slit lamp examination.
Systemic infection may be concurrent so patients should be monitored closely. Treatment consists of oral or intravenous acyclovir and topical antiviral medications, if the cornea is affected, to minimize the risk of scarring and subsequent vision loss. (9)
In addition to complete clinical examination of the neonate, conjunctival scrapings should be sent for Gram stain and culture to help identify the organism and treat it directly; This is because other bacteria such as Staphylococcus aureus , Pseudomonas and other pathogens can sometimes be the infectious organism. Depending on the clinical context, polymerase chain reaction testing, blood cultures, and/or additional evaluation for other infections may be warranted. Although the neonatologist is essential to make the diagnosis of conjunctivitis and initiate treatment, it is beneficial to involve the Ophthalmology service early in the clinical course, especially if corneal involvement is suspected.
> Cornea
Corneal clouding or opacity is associated with a wide variety of pathologies and requires consultation with ophthalmology to help determine the etiology, early treatment, and prompt evaluation of associated syndromes, if indicated.
> Trauma
Birth trauma, often involving forceps delivery, can cause vertical tears in Descemet’s membrane (posterior corneal layer), resulting in unilateral corneal clouding. Most resolve within a few months, but these babies should be followed by an ophthalmologist because this opacification can be amblyogenic if it persists and is located within the visual axis. These patients may also develop significant astigmatism, which may also be amblyogenic.
> Congenital glaucoma
The classic triad of photophobia, lacrimation, and blepharospasm is diagnostic of congenital glaucoma. Continued elevated intraocular pressure results in ruptures in Descemet’s membrane
(horizontal tears called Haab striae) and clouding of the cornea. It also leads to optic nerve damage, increased corneal diameters, and buphthalmos (enlarged eyeball) as a result of rapid elongation of axial length. Neonates with suspected congenital glaucoma require urgent referral to ophthalmology, since surgical intervention is the main treatment modality and rapid lowering of intraocular pressure can prevent and even reverse damage to the optic nerve and associated vision loss. (10)
> Corneal ulcer
Corneal ulcer presents as an infiltrative opacification with associated thinning of the cornea. Most commonly, ulcers result from infection (see Conjunctivitis section above) and require urgent ophthalmologic consultation for culture and initiation of topical antibiotic drops. Sterile ulceration may develop upon exposure related to eyelid defects, lagophthalmos, or neurotrophic cornea.
> Anterior segment dysgenesis
Anterior segment dysgenesis (ASD) encompasses several developmental disorders of the components of the anterior segment of the eye (cornea, iris, lens, and aqueous humor). Often, the presenting clinical feature is corneal opacification or clouding or other structural abnormalities of the iris or lens visible on flashlight examination.
Secondary glaucoma is common in these patients. The most common DSA disorder is Peters anomaly, which presents with variable central corneal opacity often with iris strands adherent to the posterior cornea. Sometimes the lens is also affected. At the other end of the spectrum is Peters-plus syndrome, which is a Peters anomaly with associated congenital brain defects, heart defects, and craniofacial anomalies. All patients with suspected DSA require ophthalmic evaluation and possibly a complete systemic evaluation depending on the presumed diagnosis. (eleven)
Sclerocornea is a congenital corneal opacification resulting from the ingrowth of scleral tissue into the peripheral cornea. It is a non-progressive condition and can be part of the DSA spectrum or occur in isolation.
> Metabolic cause
The most common metabolic cause of corneal opacity or clouding is mucopolysaccharidosis and its variants. This clouding is the result of the accumulation of metabolic pathway products in the cornea and presents as a bilateral diffuse corneal opacity. If a metabolic etiology is suspected, systemic evaluation is indicated. Dense cloudiness is amblyogenic, so in addition to treating the underlying disorder, the main intervention is eventual corneal surgery.
> Edema
It includes various congenital corneal dystrophies present at or occurring after birth with varying degrees of corneal opacity or clouding, generally caused by a defect in the endothelium, or most posterior corneal layer. The opacity pattern may be patchy or diffuse, and usually both eyes are affected. Most dystrophies are hereditary and are not associated with systemic disease. As in the metabolic disorders mentioned above, the mainstay of ocular intervention is surgery.
> Dermoid
A dermoid is an overgrowth of normal, benign tissue in an abnormal location. It can grow anywhere on the body, including the orbit or ocular surface. Typically, ocular surface dermoids grow at the limbus or junction of the cornea and sclera, and appear as a white nodular lesion covering a portion of the cornea. Since these can cause amblyopia if they obstruct the visual axis as well as irritation, referral to ophthalmology is justified due to possible surgical intervention.
> Coloboma of the iris
Often identified during pupil examination, iris colobomas present as an irregularly shaped pupil or iris tissue, often with a keyhole appearance. Colobomas are the result of incomplete closure of the embryonic fissure during the first weeks of development, and typically occur in the inferior nasal quadrant of the iris.
They may be sporadic in occurrence or associated with various genetic syndromes, including CHARGE syndrome (colobomas, heart defects, nasal choanal atresia, developmental restriction, genitourinary anomalies, ear and hearing anomalies) and renal coloboma syndrome among many. others, so genetic consultation is often justified. Additionally, referral to ophthalmology is indicated to evaluate colobomas or dysgenesis in other ocular structures.
> Aniridia
Aniridia refers to hypoplasia or absence of iris tissue. On examination, iris tissue may vary from the appearance of a persistently large or dilated pupil to a simple stump of the iris near the limbus. Approximately two-thirds of aniridia cases are isolated anomalies inherited in a dominant genetic manner with variable expressivity.
It is important to note that a subset of sporadic cases of aniridia are part of WAGR syndrome (Wilms tumor, aniridia, genitourinary anomalies and disability [previously known as mental retardation]) and therefore, these patients are at risk of developing a tumor by Wilms.
Additional ocular disorders associated with aniridia include foveal hypoplasia, cataracts, glaucoma, and corneal abnormalities. Therefore, referral to ophthalmology is warranted in all cases of aniridia and the visual prognosis is highly variable depending on the extent of additional structural defects. (12)
> Crystalline
Congenital cataracts can range from a small central white dot to a diffuse opacification of the lens visible on red reflex testing as a black dot or spot in the reflex to significant attenuation of the reflex or leukocoria due to blockage of the lens.
light through the opacified lens. Unilateral cataracts are typically sporadic. Persistent fetal vasculature is a type of congenital cataract associated with microphthalmia, elongation of the ciliary processes, and a stalk extending from the posterior surface of the lens to the optic nerve. Severe cases may involve retinal detachment.
Bilateral cataracts, on the other hand, are more commonly caused by an inherited genetic mutation or associated with systemic abnormalities such as metabolic disorders (galactosemia, hypocalcemia, etc.), infection (e.g., TORCH [toxoplasmosis, other agents, rubella, cytomegalovirus, and herpes simplex infections]) or syndromes such as trisomy 21. Although it is important to carry out an adequate evaluation of these cases, the majority of bilateral cataracts do not have an identifiable cause. (13)
| Posterior segment |
> Retinoblastoma
Retinoblastoma is the most common primary eye tumor in children and can affect one or both eyes. The most common presenting sign is leukocoria on the red reflex test. Retinoblastoma is discussed in detail in a separate article and is therefore not discussed further here.
> Retinopathy of prematurity
Retinopathy of prematurity (ROP) is an ocular complication related to prematurity that is distinguished by neovascularization of the retina, causing retinal detachment and blindness in the most severe cases.
Because ROP is associated with lower gestational age and birth weight, the criteria for its detection include:
1) birth weight ≤ 1,500 g,
2) gestational age ≤ 30 weeks, or
3) infants with an unstable clinical course and considered by their neonatologist/pediatrician to be at high risk for ROP. (14)
retinal hemorrhages
> Fundus hemorrhages are common among newborns, present in approximately 20% to 34% of infants. (16) (17) Hemorrhages can affect all 4 quadrants and multiple layers. They are more common in vaginal births (specifically vacuum-assisted births) compared to cesarean sections and are believed to be caused by an acute increase in intracranial pressure as the head passes through the birth canal.
They may be an incidental finding on dilated eye examination for other reasons and do not require any intervention because most cases resolve within 2 weeks of the initial finding. (17) Similarly, subconjunctival hemorrhages are also a common finding in the neonatal period after vaginal delivery or cesarean section due to elevated venous pressure in the head and neck from uterine contractions. (18)
It is important to remember that ocular hemorrhages may also be evidence of abusive head trauma in infants within an appropriate context, and this suspicion should be investigated with the appropriate subspecialty team.
> Retinal/optic nerve colobomas
Similar to iris colobomas, retinal or optic nerve colobomas result from incomplete closure of the embryonic fissure during development. The most common location is the inferior nasal quadrant of the involved structure. Depending on the size and location of the coloboma, visual acuity can vary significantly, with the associated early nystagmus being a poor prognostic sign for vision.
Posterior segment colobomas can be identified on newborn eye examination as a dull red or white reflex. Numerous syndromic and genetic abnormalities are associated with ocular colobomas so the multidisciplinary approach to evaluation and diagnosis should include the neonatologist or pediatrician, ophthalmologist, geneticist and other subspecialists, based on the findings of the clinical examination.
Although there is currently no definitive treatment for posterior segment ocular colobomas, these patients should be followed by an ophthalmologist to ensure optimization of vision through correction of refractive error, management of strabismus, and overall ocular health.
> Optic nerve hypoplasia
Optic nerve hypoplasia is characterized by a decreased number of optic nerve axons resulting in a small and often pale or gray appearing nerve. It may be a unilateral or bilateral, non-progressive finding, and the associated visual acuity may vary widely from 20/20 to no light perception.
Due to the common association with midline brain structural defects (absence of septum pellucidum, agenesis of the corpus callosum, pituitary gland dysfunction, etc.), magnetic resonance imaging (MRI) is indicated in patients with this diagnosis, as well as referral to appropriate subspecialties such as endocrinology, depending on imaging findings. (19) Similarly, findings suggestive of septo-optic dysplasia or another optic nerve abnormality on MRI should prompt referral to an ophthalmologist.
> Cortical visual impairment
Cortical (cerebral) visual impairment (CVI) is currently the leading cause of significant visual impairment in children in developed countries as a result of increased survival of preterm infants. (20) It is characterized by a decreased visual response caused by a neurological problem that affects the visual part of the brain. This may manifest as decreased visual acuity, visual field deficits, or abnormalities in visual processing.
CVD has multiple etiological factors, all of which derive from brain damage that occurs in the perinatal period or from structural abnormalities in the visual processing centers of the brain. The most common cause is hypoxic-ischemic brain injury; CVD can often coexist with other neurological disorders. Typically, these children have normal findings on anatomical examination of the eye or an ocular condition that cannot explain the degree of abnormal visual function observed. (twenty-one)
Often, visual impairment secondary to the aforementioned neurological causes is not evident at birth, but rather signs and symptoms manifest over time. In the absence of any structural or anatomical abnormality noted on careful ocular examination by the neonatologist or pediatrician that would result in more rapid referral, poor visual behavior, persistent strabismus, or abnormal eye movements beyond 3 months of age warrant evaluation. by an ophthalmologist. Early intervention with low vision services is important to help affected children optimize their visual function and overall development.
Summary
|
| Comment |
Ocular alterations in the first months of life due to a variety of structural or anatomical factors can have serious short- and long-term consequences due to altered vision development.
Therefore, ocular examination is an essential component of neonatal evaluation, as early diagnosis and referral to a specialist can have a critical impact on the prognosis of many of these ocular conditions.
Neonatologists and pediatricians should be familiar with routine visual examination and should know the most common ocular anomalies to act accordingly or make appropriate consultations.
Table 1. Differential diagnosis for abnormal red reflex.
| Location | Diagnosis |
| Previous segment | Corneal opacity congenital cataract
|
| Posterior segment (leukocoria) | Retinal detachment
Retinoblastoma
Vitreous hemorrhage
Uveitis |