Prediction of major complications in patients undergoing laparoscopic and open hysterectomy for benign indications
Hysterectomy is one of the most frequently performed surgical procedures. Canada has one of the highest hysterectomy rates in the world, with one-third of women undergoing this procedure before the age of 60. Minimal access approaches are preferred by both doctors and patients, and the proportion of hysterectomies performed using a laparoscopic approach has increased substantially in many countries over the past 10 years.
The evidence-based medicine paradigm for surgical approaches to hysterectomy for benign diseases advocates that the surgeon discuss the chosen surgical approach with the patient and decide in light of the circumstances, relative benefits and risks.
Most physicians performing a hysterectomy will intuitively identify patient characteristics that have the potential to increase the complexity and complications of the surgery. A 2016 systematic review of studies reporting significant associations between patient characteristics and surgical outcomes of laparoscopic hysterectomy and a 2020 population-based prospective cohort study using data from the Danish Hysterectomy Database suggested that Advanced age, race, high body mass index (BMI), diabetes mellitus, increased uterine weight, fibroids, endometriosis, and adhesions are predictors of complications in patients undergoing hysterectomy for benign indications.
However, assimilating this information to individualize and anticipate each patient’s precise risk if multiple factors are present can be challenging. A 2020 systematic review reported that risk prediction models outperformed surgeons in other specialties in estimating risk and postoperative results; its discriminatory ability showed greater variation (C-statistic 0.51–0.75) than other risk prediction tools.
Patients should be educated about potential risks before surgery to manage expectations. This is especially important when considering surgery for a benign disease because there are often non-surgical options available.
Our goal was to generate prediction models that can be used in conjunction with a surgeon’s intuition to improve preoperative patient counseling and match advances made in the technical aspects of surgery. We sought to quantify the proportion of patients who underwent hysterectomy for benign disease and will have a major complication, and to develop and validate prognostic models to individualize this risk, using a national data set.
Background:
Hysterectomy, the most common gynecological operation, requires surgeons to counsel women about the risks of the operation. Our objective was to develop and validate multivariable logistic regression models to predict major complications of abdominal or laparoscopic hysterectomy for benign conditions.
Methods:
We obtained routinely collected administrative health data from the English National Health Service (NHS) from 2011 to 2018. We defined major complications based on core outcomes for postoperative complications, including ureteral, gastrointestinal, and vascular injuries, and of the wound.
We specified 11 a priori predictors . We used internal-external cross-validation to assess discrimination and calibration across 7 NHS regions in the development cohort. We validated the final models using data from an additional NHS region.
Results:
We found that major complications occurred in 4.4% (3,037/68,599) of laparoscopic hysterectomies and 4.9% (6,201/125,971) of abdominal hysterectomies. Our models showed consistent discrimination in the development cohort (laparoscopic, C statistic 0.61, 95% confidence interval [CI] 0.60 to 0.62; abdominal, C statistic 0.67, 95% CI % 0.64 to 0.70) and similar or better discrimination in the validation cohort (laparoscopic, C statistic 0.67, 95% CI 0.65 to 0.69; abdominal, C statistic 0.67, 95% CI: 0.65 to 0.69).
Adhesions were the most predictive of complications in both models (laparoscopic, odds ratio [OR] 1.92, 95% CI: 1.73 to 2.13; abdominal, OR 2.46, 95% CI: 2, 27 to 2.66). Other predictors of complications included adenomyosis in the laparoscopic model and Asian ethnicity and diabetes in the abdominal model. Protective factors included age and diagnoses of menstrual disorders or benign adnexal mass in both models and diagnosis of fibroids in the abdominal model.
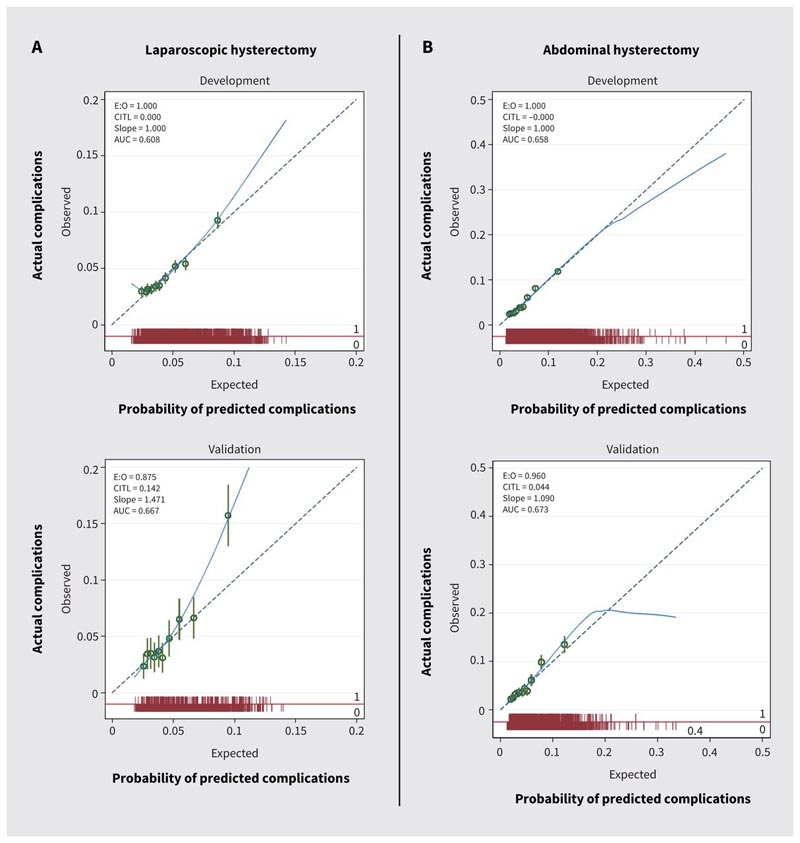
Calibration plots for the prediction of major complications in patients undergoing (A) laparoscopic or (B) abdominal hysterectomy for benign indications. Note: AUC = area under the curve, CITL = overall calibration, E = expected, O = observed.
Interpretation:
Personalized risk estimates from these models, which showed moderate discrimination, can inform clinical decision making for people with benign conditions that may require hysterectomy.
Comments
Easy-to-use tool predicts complications in patients undergoing hysterectomy for benign disease
Researchers have developed easy-to-use online prediction tools that provide personalized risk estimates for patients undergoing hysterectomy for benign disease. The study describing the models is published in CMAJ ( Canadian Medical Association Journal ).
Hysterectomy is one of the most common surgical procedures, with one-third of women in Canada undergoing this procedure before the age of 60. Laparoscopic hysterectomies are performed more frequently because they are less invasive than abdominal surgery. Current practice involves surgeons discussing the benefits of the type of procedure and the risks of complications with patients.
Researchers in the United Kingdom and Spain developed and tested prediction models with the aim of complementing a surgeon’s expert opinion about which patients might be at risk of complications from hysterectomy. Complications from hysterectomies can include ureteral, gastrointestinal, and vascular injury, as well as wound complications. The authors used data from the English National Health Service (NHS) on 68,599 women who underwent laparoscopic hysterectomies and 125,971 women who underwent abdominal hysterectomies between 2011 and 2018.
"Historically, a surgeon’s intuition has been shown to be a good indicator of postoperative outcomes; however, expert opinion is the lowest value in evidence-based medicine," says Dr. Krupa Madhvani, from Queen Mary University of London, United Kingdom. "While a surgeon’s experience and expert opinion are useful, they cannot be used alone to guide risk management. In Canada and around the world, the overall rate of hysterectomy for benign disease is declining, and more patients undergo surgery by lower-volume surgeons, who may not have experience in all procedures," the authors write.
Using 11 predictors , such as age, body mass index and diabetes, the researchers also included ethnicity as a potential risk factor, categorizing patients’ self-described ethnicity linked to a recent census.
"Ethnicity has been shown to be an independent factor influencing the route and complications of hysterectomy," the authors write.
They found that Asian women had a higher risk of serious complications after abdominal hysterectomy compared with white women, although the risk was not associated with laparoscopy. The most significant risk factor for major complications in both procedures was the presence of adhesions, which is consistent with existing evidence.
"These tools will guide shared decision-making and may lead to referral to centers with greater surgical experience or exploration of nonsurgical treatment options," the authors write.
Conclusion We have developed simple online prediction tools using routinely collected data that provide personalized risk estimates for patients undergoing hysterectomy for benign disease and that surgeons can use to assist in preoperative counseling. These tools will guide shared decision making and may lead to referral to centers with greater surgical experience or exploration of nonsurgical treatment options. Although a surgeon’s experience and expert opinion are useful, they cannot be used solely to guide risk management. In Canada and around the world, the overall rate of hysterectomy for benign disease is declining, and more patients are undergoing surgery by lower-volume surgeons, who may not be experienced in all procedures. The majority of hysterectomies in Canada are for benign indications and, with calls for continued investment in gynecologic surgery, our models could be useful tools for risk stratification. Additional research should focus on improving the discriminatory ability of these tools by including factors other than patient characteristics, including surgeon volume, as this has been shown to reduce complications. |
















