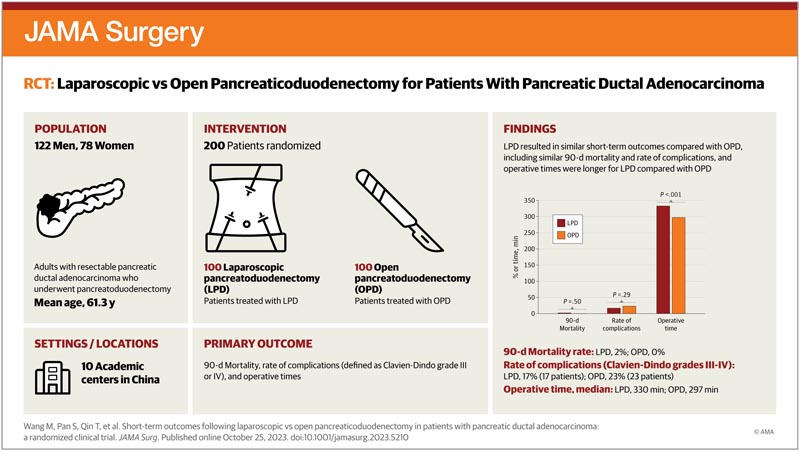
Key points Does laparoscopic pancreaticoduodenectomy performed by experienced surgeons who have overcome the learning curve produce similar short-term results as open pancreaticoduodenectomy in patients with pancreatic ductal adenocarcinoma? Findings In this randomized clinical trial that included 200 patients with pancreatic ductal adenocarcinoma, laparoscopic pancreaticoduodenectomy produced similar short-term outcomes as open pancreaticoduodenectomy , with comparable postoperative length of stay, postoperative surgical complications, number of lymph nodes removed, and mortality. to 90 days. Meaning For experienced pancreatic surgeons, performing laparoscopic pancreaticoduodenectomy in resectable pancreatic cancer was technically safe and did not increase the risk of intraoperative and postoperative complications in this study. |
Pancreatic ductal adenocarcinoma ( PDAC) remains a highly fatal malignant disease and is the third leading cause of death among adults, with an estimated 5-year survival rate of 11%. Pancreaticoduodenectomy (PD) was first developed for injuries to the head of the pancreas and has evolved over the past 100 years . With the development of minimally invasive surgery , laparoscopic PD (LPD), once known as the Mount Everest of pancreatic surgery, has seen unprecedented development in recent years. Although several reports have shown that LPD is safe, there is a paucity of studies with sufficient numbers of patients that would allow laparoscopic surgery in PDAC to be clinically accepted.
Importance
The safety and efficacy of laparoscopic pancreaticoduodenectomy for pancreatic ductal adenocarcinoma remain controversial.
Aim
To compare laparoscopic and open pancreaticoduodenectomy performed by experienced surgeons in patients with pancreatic ductal adenocarcinoma.
Design, environment and participants
This was a randomized, open-label, non-inferiority clinical trial conducted between September 20, 2019 and March 20, 2022, in 10 hospitals in China. A total of 412 adult patients were assessed for eligibility; Two hundred patients with histologically confirmed or clinically diagnosed pancreatic ductal adenocarcinoma who were eligible to undergo pancreaticoduodenectomy were enrolled.
Recruitment for the study is complete and follow-up is ongoing. This article reports the first pre-specified safety results from the trial.
Interventions
Participants were randomly assigned in a 1:1 ratio to undergo laparoscopic or open pancreaticoduodenectomy , which would be performed by experienced surgeons who had already performed at least 104 laparoscopic pancreaticoduodenectomy operations.
Main results and measures
The primary endpoint is 5-year overall survival , but the data for this endpoint are not yet mature; therefore, short-term secondary outcomes, including operative findings, complications, mortality, and oncologic outcomes, are reported here. Results were analyzed according to a modified intention-to-treat and per-protocol principle.
Results
Among 412 eligible patients, 200 patients were enrolled and randomly assigned 1:1 to undergo laparoscopic pancreaticoduodenectomy or open pancreaticoduodenectomy . The mean (SD) age was 61.3 (9.3) years and 78 participants (39%) were women.
Laparoscopic procedures had longer operative times (median [IQR], 330.0 [287.5-405.0] minutes vs. 297.0 [245.0-340.0] minutes; P < .001).
Patients in the laparoscopic group lost less blood than those in the open group (median [IQR], 145.0 [100.0-200.0] mL vs. 200.0 [100.0-425.0] mL; P = .02).
Ninety-day mortality occurred in 2 of 100 patients in the laparoscopic group and 0 of 100 patients in the open group .
There were no differences in complication rates for Clavien-Dindo grades III-IV (n = 17 [17.0%] vs. n = 23 [23.0%]; P < ai = 7 > = .29), comprehensive complication rate (median [IQR], 0.0 [0.0-22.6] vs 8.7 [0.0-26.2]; P = .79) or median (IQR) duration of postoperative stay (14.0 [11.0-17.0] days vs. 14.0 [12.0-18.5] days; P = .37) between the 2 groups.
Conclusions and relevance Laparoscopic pancreaticoduodenectomy performed by experienced surgeons at high-volume specialty institutions produced similar short-term outcomes compared with open pancreaticoduodenectomy among patients with pancreatic ductal adenocarcinoma. |
Trial Registration ClinicalTrials.gov Identifier: NCT03785743
















