The incidence of inflammatory bowel disease (IBD) is increasing significantly in developing and newly developed countries, particularly in children and older age groups, contributing to aggravated prevalence.
The objective of this review is to discuss the implications of changing trends in the epidemiology of IBD. These patterns provide information about causes as they occur concurrently with changes in the environment. Furthermore, we must prepare for the growing burden of IBD and address it at multiple levels, guided by disease prevention principles.
| Understanding non-genetic risk factors for IBD |
There is marked heterogeneity in risk variants across populations and limited concordance within families, even among monozygotic twins. The rise of IBD has paralleled industrialization and major changes in the environment.
Migration from a developing country to a Western country is associated with an increased risk of IBD and other immune-mediated diseases. These indirect data corroborate the role of non-genetic factors. They are classified into factors related to the environment, lifestyle and health ( Figure 1 ).
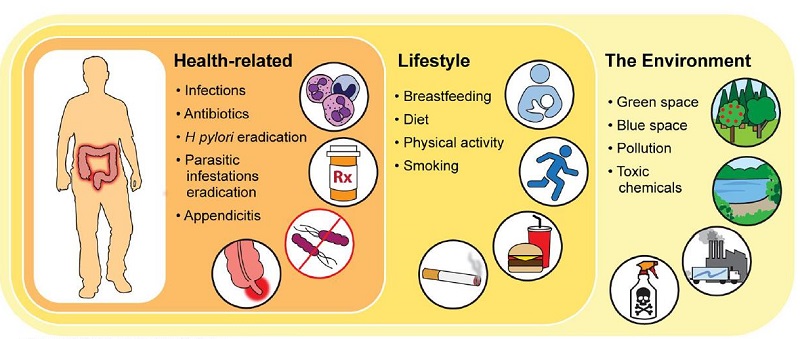
FIGURE 1. Risk factors related to the environment, lifestyle and health involved in the risk of IBD. IBD, inflammatory bowel disease.
> The environment
Early exposure to pollution was associated with later risk of IBD. Residential green spaces during the early life period were found to protect against IBD in a dose-dependent manner. These data are consistent with other reports on the protective effect of green spaces on health and mortality.
The mechanisms through which environmental health may be causally related to human health are not well elucidated, but improved immune tolerance, lower levels of stress, improved diet and physical activity, and exposure to pollutants may be some potential mechanisms.
> Lifestyle
Breastfeeding influences the immune modulation of children, the establishment of the microbiome and the risk of many chronic diseases. Additionally, formula foods, the typical alternative to breastfeeding, contain emulsifiers and other synthetic molecules, which are involved in intestinal inflammation and host-microbe interactions.
Recent data have corroborated the role of modern and urban diets in IBD. Consumption of ultra-processed foods was associated with IBD in a dose-dependent manner. In contrast, the Mediterranean diet, which is rich in healthy, naturally occurring foods such as vegetables, fruits, fish and nuts, protected against Crohn’s Disease (CD).
Other lifestyle factors such as smoking, stress, anxiety and lack of physical activity, which are ingrained in modern, urban society, are also implicated in the risk of IBD.
> Health related
Infections have been linked to IBD risk in all studies, particularly gastrointestinal bacterial infections such as Salmonella and Campylobacter. On the contrary, Helicobacter pylori may have a protective role against IBD. H. pylori eradication was associated with an increased risk of immune-mediated diseases, including IBD.
Antibiotic use in all age groups has been associated with an increased risk of IBD in a dose-dependent manner. These data imply the alteration of the intestinal microbiome.
Appendectomy at age <20 years for appendicitis or mesenteric lymphadenitis was associated with a lower risk of Ulcerative Colitis (UC). Furthermore, appendicitis and appendectomy are also reported to modulate the course of UC.
> Timing of exposure: early life period versus later in life
The early life period, extending from prenatal to early childhood, is a critical window for immune development and establishment of the microbiome. Exposures during this period confer a lasting effect on offspring. This hypothesis, known as the developmental origins of health and disease, is relevant to IBD.
| Response to increased burden of IBD |
IBD is a life-course disease, often occurring in children and young adults, and has no cure. It is associated with complications such as infections, hospitalizations, surgeries and cancer. It leads to an adverse impact on mental health and disability. Treatment of IBD involves long-term use of biologics and complex surgeries, each of which incurs significant healthcare costs.
As the incidence and prevalence of IBD continues to rise, even and especially in developing countries, the urgency of preparing healthcare systems and mitigating its impact cannot be underestimated.
In this article, the principles of disease prevention are applied, analogous to what is done in other chronic pathologies such as diabetes and cardiovascular diseases, to control the impact of IBD. The discussion begins with tertiary prevention, a goal widely achieved, and we move towards primary prevention, to which we aspire ( Figure 2 ).
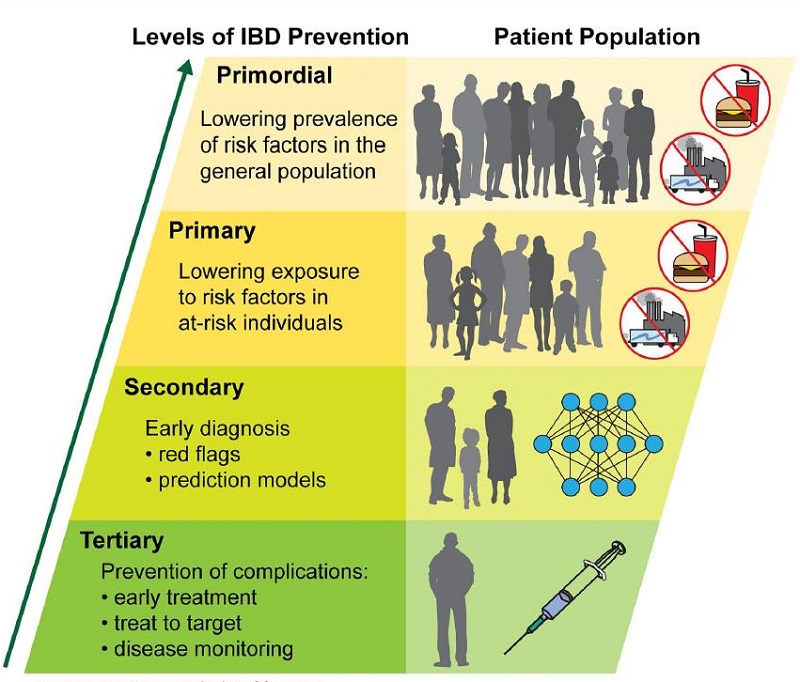
FIGURE 2. IBD prevention levels.
> Tertiary prevention: early treatment of IBD
Strong data demonstrate that early treatment of IBD is essential to prevent complications. Biologic therapy within 2 years of diagnosis was associated with higher rates of remission and mucosal healing compared with delayed or nonbiologic treatment.
Like CD, UC is also a progressive disease; Although data on long-term outcomes with early treatment are lacking, it is reasonable to institute early and appropriate intervention to reduce the risk of colectomy and colorectal cancer.
> Secondary prevention: Early diagnosis of IBD
Early diagnosis, an essential step for timely treatment, is of great relevance. CD can be associated with varied and non-specific symptoms, leading to a delay in the identification of the condition.
To minimize delay in diagnosis, the Red Flag Index, a questionnaire of relevant signs and symptoms, was developed. This, in combination with fecal calprotectin, has been validated as a tool for early diagnosis of CD.
> Primary prevention: Reduction in the risk of IBD among individuals at risk
Primary prevention involves reducing the risk among at-risk individuals, thus preventing the onset of the disease. The genetic risk of IBD, represented by family history, is considered one of the most important factors.
People with immune-mediated diseases such as lupus, rheumatoid arthritis, and ankylosing spondylitis are at risk for IBD. Parental history of an immune-mediated disease is also a factor to consider.
The next step in primary prevention is to identify an intervention to prevent the onset of IBD in at-risk individuals. The key characteristics of such an action would be safety, effectiveness and ease of administration.
> Primary prevention: reduction in the prevalence of risk factors
Finally, the general objective would be to apply prevention principles to the general population and work to reduce the prevalence of risk factors for IBD and other chronic diseases. It would be necessary to restrict the use of fuels, minimize pollution, implement sustainable practices and fight climate change.
These efforts are required at the individual, societal, national and global levels. Relatedly, lifestyle changes such as healthy diets, minimizing the intake of processed foods, avoiding smoking, and spending time in nature would be considerations, not only in the context of IBD, but also for improving overall health. general.
| Conclusion |
The evolution of IBD epidemiology on a global scale provides important information on the risk and pathogenesis of the pathology. Environmental health is closely related to IBD risk and outcomes, as with other chronic diseases. As the burden of IBD changes, we must prepare global health systems to mitigate its impact.















