Highlights
|
Summary
Importance
Menopause is defined as the cessation of a person’s menstrual cycle. It is defined retrospectively, 12 months after the last menstrual period. Perimenopause, or the menopause transition, is the period of a few years preceding a person’s last menstrual period and is characterized by increased variability in the length of the menstrual cycle and periods of amenorrhea and often symptoms such as dysfunction vasomotor. The prevalence and incidence of most chronic diseases (e.g., cardiovascular disease, cancer, osteoporosis, and fractures) increase with age, and Americans who reach menopause are expected to live on average for more than another 30 years. .
Aim
To update its 2017 recommendation, the US Preventive Services Task Force ( USPSTF ) commissioned a systematic review to evaluate the benefits and harms of systemic (i.e., oral or transdermal) hormone therapy ) for the prevention of chronic conditions in postmenopausal people and whether results vary by age or timing of intervention after menopause.
Population
Asymptomatic postmenopausal people who are considering hormone therapy for the primary prevention of chronic medical conditions.
Evaluation of the evidence
The USPSTF concludes with moderate certainty that the use of combined estrogen and progestin for the primary prevention of chronic conditions in postmenopausal people with an intact uterus has no net benefit. The USPSTF concludes with moderate certainty that the use of estrogen alone for the primary prevention of chronic conditions in postmenopausal people who have had a hysterectomy has no net benefit .
Recommendation
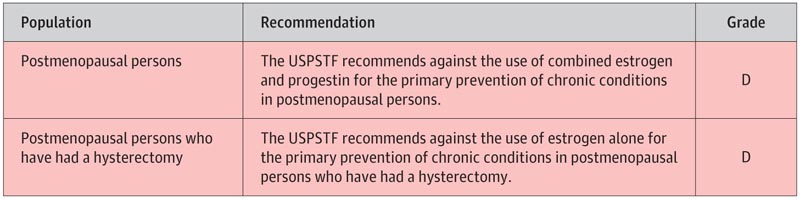
- The USPSTF recommends against the use of combined estrogen and progestin for primary prevention of chronic conditions in postmenopausal people.
- (Recommendation D) The USPSTF recommends against the use of estrogen alone for primary prevention of chronic conditions in postmenopausal people who have had a hysterectomy. (Recommendation D)
Summary of recommendations
Importance
Menopause is defined as the cessation of a person’s menstrual cycle. It is defined retrospectively, 12 months after the last menstrual period. Perimenopause , or the transition to menopause, is the period of a few years preceding a person’s last menstrual period and is characterized by increased variability in the length of the menstrual cycle and periods of amenorrhea and often symptoms such as dysfunction vasomotor. Natural menopause occurs at an average age of 51.3 years.
The prevalence and incidence of most chronic diseases (e.g., cardiovascular disease, cancer, osteoporosis, and fractures) increase with age, and Americans who reach menopause are expected to live longer on average than others. 30 years. However, the excess risk of chronic diseases that can be attributed to menopause alone is uncertain.
Assessing the magnitude of the USPSTF net benefit
The US Preventive Services Task Force ( USPSTF ) concludes with moderate certainty that there is no benefit from the use of combined estrogen and progestin for the primary prevention of chronic conditions in postmenopausal people with an intact uterus. net .
The USPSTF concludes with moderate certainty that the use of estrogen alone for the primary prevention of chronic conditions in postmenopausal people who have had a hysterectomy has no net benefit .
Considerations for practice
Patient population under consideration
This recommendation statement applies to asymptomatic postmenopausal individuals who are considering hormone therapy for the primary prevention of chronic medical conditions. It does not apply to people who are considering hormone therapy to control perimenopausal symptoms, such as hot flashes or vaginal dryness. It also does not apply to people who have had premature menopause (primary ovarian failure) or surgical menopause.
Trials that provided evidence on the benefits and harms of menopausal hormone therapy for this recommendation generally used the term "women" to describe participants, although it is likely that these trials enrolled participants on the basis of sex, not of gender identity.
Other Related USPSTF Recommendations
The USPSTF has made several recommendations related to the prevention of cardiovascular disease and other chronic conditions in adults, including the use of aspirin for the prevention of cardiovascular disease, screening for high blood pressure, screening for prediabetes and type 2 diabetes, behavioral counseling to promote healthy eating and physical activity for the prevention of cardiovascular disease in adults (with and without cardiovascular risk factors) and screening for osteoporosis. The USPSTF has also made recommendations on breast cancer screening and colorectal cancer screening.
Update to previous USPSTF recommendation
This recommendation replaces the 2017 USPSTF recommendation on hormone therapy for primary prevention of chronic conditions in postmenopausal women. In 2017, the USPSTF recommended against the use of combined estrogen and progestin for the primary prevention of chronic conditions in postmenopausal women and against the use of estrogen alone for the primary prevention of chronic conditions in postmenopausal women who have had a hysterectomy. This recommendation is consistent with the 2017 USPSTF recommendation.
Benefits and harms of preventive medication
The USPSTF found 20 randomized clinical trials that compared the effects of estrogen, either alone or in combination with progestin, versus placebo for the prevention of chronic conditions. Of these studies, the WHI trials were the only studies powered to evaluate the effectiveness of hormone therapy for the primary prevention of various chronic conditions. The WHI trials included postmenopausal people aged 50 to 79 years; The average age of the participants was 63 years. The WHI compared 0.625 mg/d oral conjugated equine estrogen, with or without 2.5 mg/d medroxyprogesterone acetate, with placebo.
Evidence on other types, doses or modes of administration of hormone therapy was limited. The WHI also had the longest duration of follow-up, with a median intervention time of 7.2 years for the estrogen-only trial and 5.6 years for the estrogen plus progestin trial, as well as long-term follow-up of up to 20. 4 years.
Recommendations from other institutions
The American College of Obstetricians and Gynecologists recommends against using menopausal hormone therapy for primary and secondary prevention of coronary heart disease. It also notes that evidence suggests that women in early menopause who have good cardiovascular health and low risk of adverse cardiovascular outcomes should be considered candidates for the use of estrogen therapy or conjugated equine estrogen plus a progestin for relief of symptoms of menopause and that menopausal hormone therapy is approved for use in women with an increased risk of osteoporosis and fractures.
The North American Menopause Society recommends that hormone therapy not be prescribed for the prevention of chronic diseases. It also notes that extended duration of use of hormone therapy may be appropriate in symptomatic women or for prevention of osteoporosis if alternative therapies are not tolerated, based on careful assessment of individual benefits and risks.
The American Academy of Family Physicians supports the USPSTF’s previous recommendation on hormone therapy in postmenopausal people.















