Heart failure (HF) affects around 1 million people in the UK and accounts for between 3% and 4% of NHS spending. Effective management improves the quality and length of life for patients, but establishing a diagnosis can be challenging due to overlapping symptoms (such as shortness of breath, exhaustion, or swollen ankles) with other conditions.
Natriuretic peptides ( NPs) are released by the myocardium in response to pressure or fluid overload and act both in the vasculature to relax smooth muscle and in the kidney to induce diuresis. NP levels are elevated in people with heart failure and testing can help with diagnostic decision making. Guidelines recommend referral for cardiac imaging and specialist evaluation based on NP level. Two types of NP tests, B-type NP (BNP) and NT-proBNP, are currently available in clinical practice. BNP is biologically active and has a shorter half-life, making it less stable over time.
The European Society of Cardiology (ESC) and the National Institute for Health and Care Excellence (NICE) recommend PN testing in acute and chronic HF.
The threshold values to rule out a diagnosis of acute heart failure in an emergency department are consistent across all guidelines (BNP <100 pg/mL and NT-proBNP <300 pg/mL) and are supported by a large body of evidence. However, the thresholds of the ESC and NICE guidelines differ by more than threefold in chronic HF . These patients present to primary care with a gradual onset of symptoms and NP testing is useful to inform the referral process.
The ESC recommends referral for echocardiography and specialist assessment of BNP ≥35 pg/ml or NT-proBNP ≥125 pg/ml while NICE recommends a higher cut-off level of BNP ≥100 pg/ml or NT-proBNP ≥400 pg/ml. ml. There is limited evidence on the optimal diagnostic threshold of PN for primary care, and current guidelines rely on small diagnostic accuracy studies, screening substudies, and consensus to make recommendations.
The aim of this study was to report the real-world diagnostic performance of NP tests for the diagnosis of chronic HF at the ESC and NICE referral thresholds.
Background
Natriuretic peptide (NP) testing is recommended for patients presenting to primary care with symptoms of chronic heart failure (HF) to prioritize referral for diagnosis.
Aim
To report NP test performance at the reference thresholds of the European Society of Cardiology (ESC) and National Institute for Health and Care Excellence (NICE) guidelines.
Design and environment
Diagnostic accuracy study using linked primary and secondary care data (2004 to 2018).
Method
The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of NP tests for the diagnosis of HF were evaluated.
Results
In total, 229,580 patients had a NP trial and 21,102 (9.2%) were diagnosed with HF within 6 months. The ESC NT-proBNP ≥125 pg/ml threshold had a sensitivity of 94.6% (95% confidence interval [CI] = 94.2 to 95.0) and a specificity of 50.0% (95% CI). % = 49.7 to 50.3), compared with a sensitivity of 81.7% (95% CI = 81.0 to 82.3) and specificity of 80.3% (95% CI = 80, 0 to 80.5) for the NICE NT-proBNP threshold ≥400 pg/mL.
The PPVs for an NT-proBNP test were 16.4% (95% CI = 16.1 to 16.6) and 30.0% (95% CI = 29.6 to 30.5) for the thresholds ESC and NICE, respectively.
For both guidelines, almost all patients with an NT-proBNP level below the threshold had no CI (NPV: ESC 98.9%, 95% CI = 98.8 to 99.0 and NICE 97.7%, 95% CI = 97.6 to 97.8).
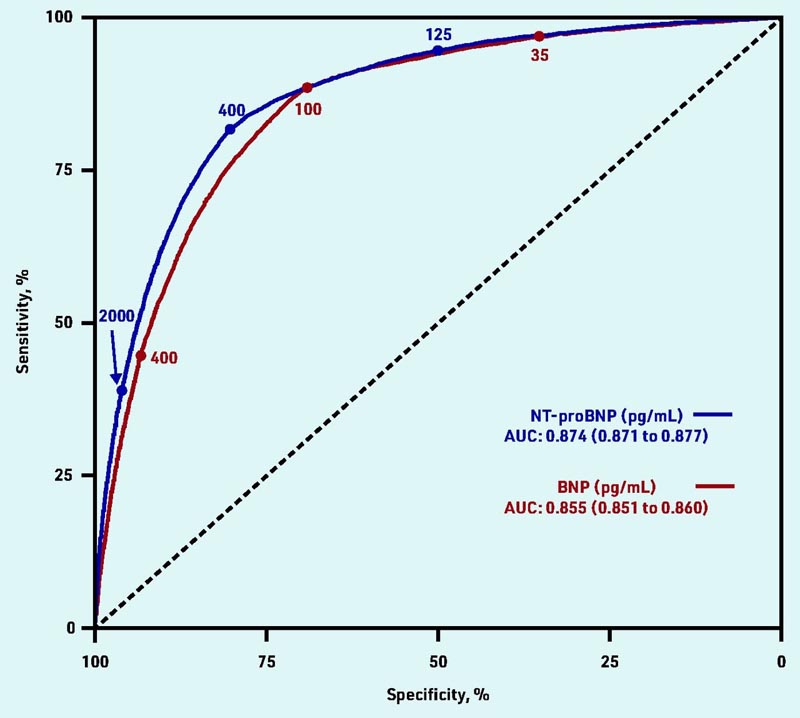
ROC curve for the diagnosis of HF for BNP and NT-proBNP tests at the ESC and NICE reference thresholds. AUC = area under the ROC curve. BNP = NP type B. ESC = European Society of Cardiology. HF = heart failure. NICE = National Institute for Health and Care Excellence. NP = natriuretic peptide. ROC = receiver operating characteristic.
Conclusion
At the higher PN thresholds of the NICE chronic HF guideline, one in five cases are initially missed in primary care, but the lower ESC thresholds require further diagnostic assessments. NP is a reliable “rule out” test at both cutoff points. The optimal PN threshold will depend on the priorities and capacity of the health system.
Summary In this large real-world diagnostic accuracy study in 229,580 primary care patients undergoing PN testing, the ESC chronic HF referral threshold of NT-proBNP ≥125 pg/mL had high sensitivity (94.6% , 95% CI = 94.2 to 95.0), but low specificity (50.0%, 95% CI = 49.7 to 50.3) compared with moderate sensitivity (81.7%, 95% CI = 49.7 to 50.3) 95% = 81.0 to 82.3) and moderate specificity (80.3%, 95% CI = 80.0 to 80.5) for the NICE NT-proBNP reference threshold ≥400 pg/mL. At NICE’s current threshold, one in five cases of HF are initially missed by NP testing; However, for each additional new diagnosis of HF at the lower ESC cut-off point, around 20 additional patients require diagnostic evaluation. Both guidelines accurately ruled out HF (NPV for ESC 98.9%, 95% CI = 98.8 to 99.0 and NICE 97.7%, 95% CI = 97.6 to 97.8) . |
Implications for research and practice
The current study suggests that at the current NICE threshold, one in five cases are initially missed after NP testing in primary care and diagnosed via an alternative route within 6 months. However, for each additional case of HF detected at the lower ESC threshold, around 20 additional patients would need to be referred for echocardiography and specialist evaluation.
Therefore, the optimal NP threshold for referral for HF diagnosis will depend in part on capacity within the healthcare setting. Patients with very high NP levels have worse outcomes and require timely referral for diagnosis and initiation of treatment, and this could be hampered if diagnostic services are overwhelmed by a lower NP referral threshold.
In the current study, an NP value below the ESC or NICE thresholds effectively ruled out HF and this may be extremely valuable in aiding diagnostic decision making in primary care.
This balance between ensuring capacity is not breached in outpatient clinics versus missing a heart failure diagnosis is a challenge for both the referring primary care physician and the heart failure specialist. When the patient has only mild symptoms and a PN level below the threshold, follow-up in primary care may be necessary.
The current study also found that people with risk factors (former smoker, hypertension, high cholesterol) and established cardiovascular disease were more likely to receive an NP trial, suggesting that doctors are targeting testing at those considered with increased risk of heart failure. In practice, NP levels are dynamic and will vary in relation to a variety of factors , including weight status, kidney function, age, and atrial fibrillation. Although current ESC and NICE guidelines have maintained the current NP thresholds used in this analysis, a recent ESC position paper on the use of NP testing suggested that some of these variables, particularly obesity, should be taken into account. account when interpreting the results.
Additional research could help refine reference thresholds for these key subgroups to help inform future guidance. In the meantime, primary care physicians should be aware that if national guidelines recommend higher PN thresholds for specialist evaluation , patients with results just below this level may still require referral for evaluation. diagnostic. Retesting PN results over time in symptomatic patients may also help improve the sensitivity of the tests and help minimize delays in the diagnosis of heart failure .
















