Survival and Healthcare Costs After Elective Inpatient Surgery: Comparison of Patients With and Without Chronic Obstructive Pulmonary Disease
Summary
Background:
Chronic obstructive pulmonary disease (COPD) is common among surgical patients, and patients with COPD have an increased risk of complications and death within 30 days of surgery. We sought to describe the longer-term postoperative survival and costs of patients with COPD compared to those without COPD within 1 year after elective inpatient surgery.
Methods:
In this population-based retrospective cohort study, we used linked health administrative databases to identify all patients who underwent elective inpatient surgery in Ontario, Canada, from 2005 to 2019. We determined COPD status using validated definitions.
We followed participants for 1 year after surgery to assess survival and costs to the healthcare system. We quantified the association of COPD with survival (Cox proportional hazards models) and costs (linear regression model with log-transformed costs) with partial adjustment (for sociodemographic factors and type of procedure) and full adjustment (also adjusting for comorbidities ). Effect modification by frailty, cancer, and type of procedure was assessed.
Results:
932,616 patients were included , of which 170,482 (18%) had COPD.
Regarding the association with the risk of death, COPD had a partially adjusted hazard ratio (HR) of 1.61 (95% confidence interval [CI], 1.58–1.64) and a fully adjusted 1.26 (95% CI 1.24–1.29).
With respect to the impact on health system costs, COPD was associated with a partially adjusted relative increase of 13.1% (95% CI 12.7%–13.4%) and an increase of 4.6% ( 95% CI 4.3%–5.0%) with full adjustment.
Frailty, cancer, and type of procedure (such as orthopedic and lower abdominal surgery) modified the association between COPD and outcomes.
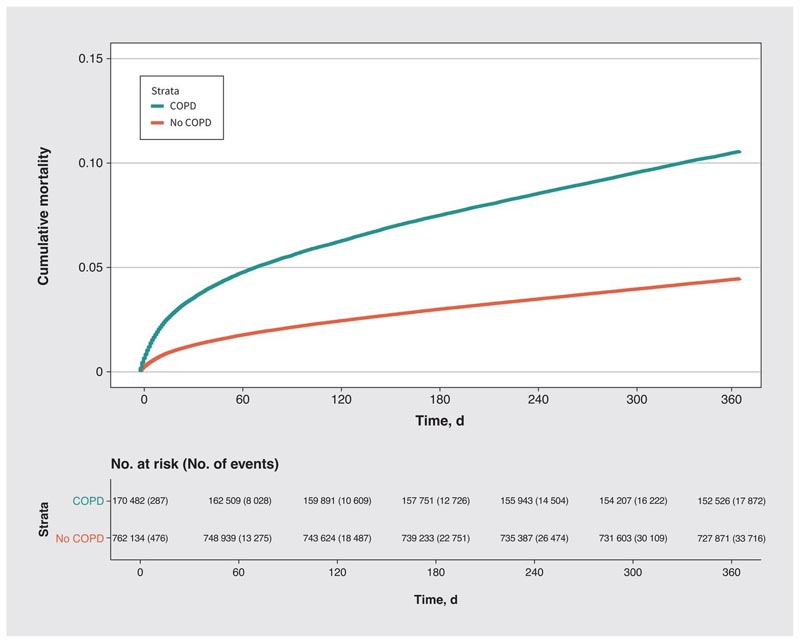
Unadjusted cumulative mortality over one year after surgery by chronic obstructive pulmonary disease (COPD) status among patients undergoing elective in-hospital surgery.
Interpretation: Patients with COPD have lower survival and higher costs in the year after surgery. Frailty, cancer, and type of surgical procedure modified the associations between COPD and outcomes and should be considered when risk stratifying surgical patients with COPD. Contemporary estimates suggest that more than 10% of surgical patients have COPD. Patients with COPD have an increased risk of complications and death within 30 days after surgery; Previous work estimates a 35% increase in the odds of morbidity and a 30% increase in the odds of death attributable to COPD after risk adjustment. However, existing studies have substantial shortcomings. Several included selected hospitals, limiting generalizability, while others were limited in scope and studied selected surgical procedures; most did not follow patients for more than 30 days after surgery. Patients with COPD may be at increased long-term risk due to age and other comorbidities. Understanding the long-term outcomes of surgical patients with COPD is critically important to accurately guide informed consent discussions and project care needs. The costs to health systems to care for COPD patients after surgery are also unknown; Delineating these costs would facilitate budgeting and resource allocation at the system level. We sought to compare survival and health care costs up to 1 year after elective inpatient surgery between patients with and without COPD in a large real-world surgical population in a health system where hospital and medical care are funded by the government. |
Comments
Patients with chronic obstructive pulmonary disease (COPD) who undergo major surgery are more likely to die in the year after surgery and incur higher healthcare costs than similar patients without COPD, a new published study found. in CMAJ (Canadian Medical Association Journal) .
"Because COPD patients are often frail and have many health problems, their management at the time of surgery must address not only COPD but all of their health problems," says Dr. Ashwin Sankar, anesthesiologist. from St. Michael’s Hospital, a Unity Health Toronto site and the University of Toronto.
The study included 932,616 patients aged 35 years and older in Ontario who underwent major surgery, including total hip or knee replacement, gastrointestinal surgery, vascular surgery and other elective non-cardiac surgeries. Of all patients, approximately 1 in 5 (170,482) had COPD. Patients with COPD were older and more likely to be male, frail, have lower incomes, and have preexisting conditions such as coronary artery disease, diabetes, and lung cancer.
Researchers found that compared to demographically similar patients without COPD who underwent similar surgery, people with COPD had a 61% higher risk of dying and a 13% increase in health care costs in the year after surgery. Surgery. These increased risks and costs were evident well after the immediate 30-day postoperative period.
"Patients with COPD often have concurrent comorbidity, biopsychosocial problems, and frailty," the authors write. "Our findings highlight the importance of careful risk prediction and decision making for COPD patients considering surgery."
They hope their findings of increased healthcare costs will help with system-level planning by policymakers and hospital administrators to better respond to the postsurgical needs of people with COPD.
















