Multicenter trial of more than 12,000 orthopedic trauma patients likely to change standard of care
Background
Clinical guidelines recommend low-molecular-weight heparin for thromboprophylaxis in patients with fractures, but trials of its efficacy compared with aspirin are lacking.
Methods
In this pragmatic, multicenter, randomized, noninferiority trial, we recruited patients 18 years of age or older who had a fracture of an extremity (anywhere from the hip to the midfoot or from the shoulder to the wrist) who had been treated surgically or who had any pelvic or acetabular injury.
Patients were randomly assigned to receive low-molecular-weight heparin (enoxaparin) at a dose of 30 mg twice daily or aspirin at a dose of 81 mg twice daily while in the hospital.
After hospital discharge, patients continued to receive thromboprophylaxis according to the clinical protocols of each hospital. The primary outcome was death from any cause at 90 days. Secondary outcomes were nonfatal pulmonary embolism, deep vein thrombosis, and hemorrhagic complications.
Results
A total of 12,211 patients were randomly assigned to receive aspirin (6101 patients) or low molecular weight heparin (6110 patients). Patients had a mean (±SD) age of 44.6±17.8 years, 0.7% had a history of venous thromboembolism, and 2.5% had a history of cancer.
Patients received a mean of 8.8±10.6 doses of in-hospital thromboprophylaxis and were prescribed a median 21-day supply of thromboprophylaxis at discharge. Death occurred in 47 patients (0.78%) in the aspirin group and 45 patients (0.73%) in the low-molecular-weight heparin group (difference, 0.05 percentage points; 96% confidence interval). .2%, −0.27 to 0.38; P < 0.001 for a non-inferiority margin of 0.75 percentage points).
Deep vein thrombosis occurred in 2.51% of patients in the aspirin group and 1.71% of those in the low-molecular-weight heparin group (difference, 0.80 percentage points; 95% CI, 0 .28 to 1.31).
The incidence of pulmonary embolism (1.49% in each group), bleeding complications, and other serious adverse events was similar in the two groups.
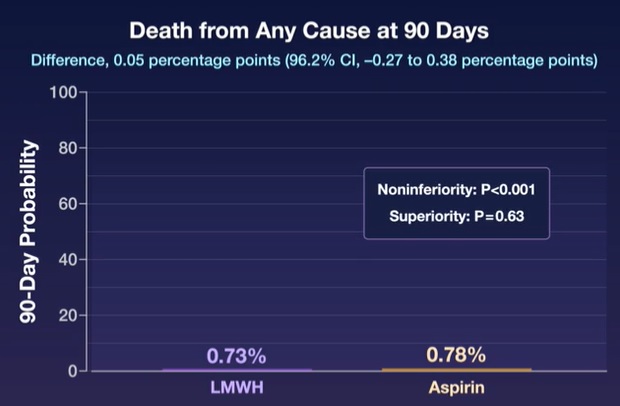
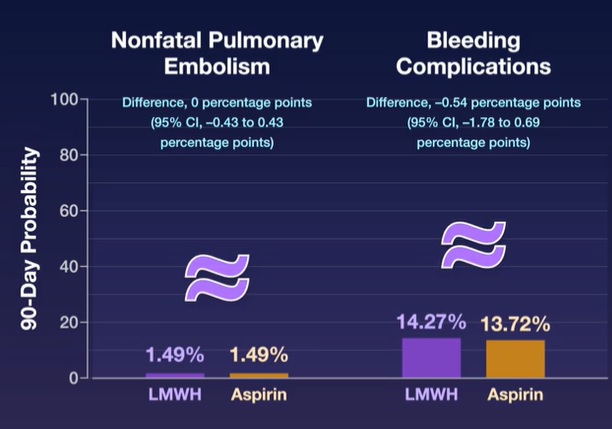
Conclusions In patients with extremity fractures who had been treated surgically or with any pelvic or acetabular fracture, thromboprophylaxis with aspirin was noninferior to low molecular weight heparin in preventing death and was associated with low incidences of deep vein thrombosis and pulmonary embolism and low 90 -daily mortality. |
(Funded by the Patient-Centered Outcomes Research Institute; PREVENT CLOT ClinicalTrials.gov number, NCT02984384. opens in new tab.)
Comments
Patients hospitalized with fractures usually receive an injectable anticoagulant, low molecular weight heparin, to prevent life-threatening blood clots. However, a new clinical trial found that cheap over-the-counter aspirin is just as effective. The findings, published in The New England Journal of Medicine , may lead surgeons to change their practice and give aspirin to these patients.
The multicenter randomized clinical trial, which included more than 12,000 patients at 21 trauma centers in the U.S. and Canada, is the largest trial ever conducted in orthopedic trauma patients. This multidisciplinary collaboration between orthopedic and trauma surgeons highlights the importance of evaluating techniques used to prevent postsurgical complications, such as blood clots and infections, through high-quality head-to-head studies.
The trial was co-led by the Department of Orthopedics at the University of Maryland School of Medicine (UMSOM) and the Major Extremity Trauma Research Consortium (METRC) based at the Johns Hopkins Bloomberg School of Public Health.
"Many fracture patients will likely prefer to take daily aspirin rather than receive injections after we found that both give them similar results for preventing the more serious outcomes of blood clots," said the study’s principal investigator, Robert V. O’Toole, MD, Hansjörg Wyss Medical Foundation Professor of Orthopedic Trauma at UMSOM and Chief of Orthopedics at the R Adams Cowley Shock Trauma Center at the University of Maryland Medical Center (UMMC). “We hope that our findings from this large-scale trial will have an important impact on clinical practice that may even alter the standard of care.”
Blood clots cause up to 100,000 deaths in the U.S. each year, according to the U.S. Centers for Disease Control (CDC). Patients who experience fractures that require surgery are at increased risk of developing blood clots. blood in the lungs and extremities. Large clots in the lungs can even be life-threatening. Current guidelines recommend prescribing low-molecular-weight heparin (enoxaparin) to prevent these clots, although smaller clinical trials in total joint replacement surgery suggested a potential benefit of aspirin as a less expensive and widely available option.
The study enrolled 12,211 patients with leg or arm fractures requiring surgery or pelvic fractures regardless of treatment. Half were randomly assigned to receive 30 mg. of low molecular weight heparin for injection twice a day. The other half received 81 mg. of aspirin twice a day. Patients were followed for 90 days to measure the health outcomes of the two treatments.
The study’s main finding was that aspirin was "noninferior" or worse than low-molecular-weight heparin in preventing death from any cause: 47 patients in the aspirin group died, compared with 45 patients in the aspirin group. of heparin. For other major complications, the researchers also found no difference between the two groups in clots in the lungs (pulmonary embolism). The incidence of bleeding complications, infections, wound problems and other adverse events of the treatments was also similar in both groups.
Of all the outcomes studied, the only potential difference seen was in deep vein thrombosis . This condition was relatively uncommon in both groups, occurring in 2.5 percent of patients in the aspirin group and 1.7 percent of patients in the heparin group.
"This relatively small difference was driven by clots in the lower leg, which are thought to be of less clinical significance and often do not require treatment," said the study’s principal investigator, Deborah Stein, MD, MPH, Professor. of Surgery at UMSOM and Director of Adult Intensive Care Services at UMMC.
The $11.7 million study was funded by the Patient-Centered Outcomes Research Institute (PCORI), (PCS-1511-32745), an independent nonprofit organization that funds comparative clinical effectiveness research to help patients. and physicians to make better-informed healthcare decisions. .
"This large multicenter study was necessary to adequately measure the impact of prophylaxis on the rare but important outcome of death that is of utmost importance to patients," said study methods center principal investigator Renan Castillo. PhD, Professor of Health Policy and Management. at the Johns Hopkins Bloomberg School of Public Health.
The trial was called PREVENTION of Clots in Orthopedic Trauma, or PREVENT CLOT. Patients enrolled in the trial were treated at the R Adams Cowley Shock Trauma Center at UMMC and 20 other trauma centers in 15 other states, as well as two in Canada. Recruitment began in April 2017 and continued until 2021.
“Many patients don’t like getting injections. It’s not fun in terms of giving the actual shot because it burns, and the stomach tends to bruise more easily compared to aspirin,” said Debra Marvel, a 53-year-old woman from Columbia, MD, who served as a patient advisor. in studying. She received Lovenox (low molecular weight heparin) after her legs were crushed in a pedestrian accident in 2015, requiring multiple surgeries at the University of Maryland Shock Trauma Center. “Patients also prefer aspirin because Lovenox can be expensive depending on insurance.”
"An estimated one million Americans are hospitalized each year with limb fractures, and this new finding could help prevent potentially fatal blood clots in these patients using a medication that is cheaper and much easier to administer," said Mark T. Gladwin, MD, Vice President for Medical Affairs at the University of Maryland, Baltimore, and the John Z. and Akiko K. Bowers Distinguished Professor and Dean of the University of Maryland School of Medicine. "Given these important results, we can expect that blood clot prevention guidelines will be revised to include the aspirin option for patients with traumatic bone fractures."
















