Executive Summary Following the 2014-2016 Ebola outbreak in West Africa and the current global COVID-19 pandemic, the One Health approach (bridging the interface between animal, environmental and human health) has rapidly gained political and financial support, in particular in regional and transcontinental countries with initiatives to improve Global Health Security, including through newly established institutions such as Africa CDC and other multidisciplinary consortia. This Lancet series of four articles explores the adoption of One Health approaches to improve health security and includes an analysis of the current landscape of preventive, surveillance and response measures in situations of outbreaks of emerging and re-emerging zoonotic infectious diseases with epidemic potential as well. as well as other potential public health emergencies, such as neglected endemic diseases, antimicrobial resistance, environmental and chemical hazards, and natural disasters. |
Fundamentals (editorial)
The notion that the well-being of an individual is directly connected to the well-being of the land has a long history in indigenous societies.
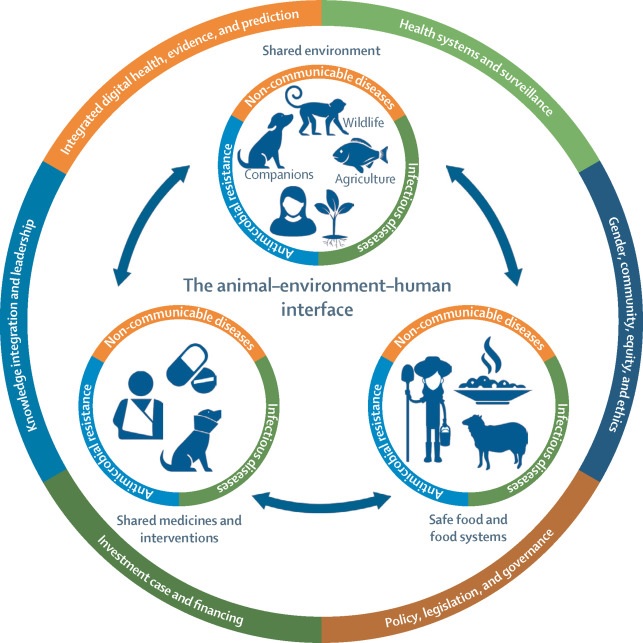
Today, the term One Health has become an important concept in global health. The One Health High-Level Expert Panel defines One Health as “an integrated and unifying approach that aims to sustainably balance and optimize the health of people, animals and ecosystems. It recognizes that the health of humans, domestic and wild animals, plants and the wider environment (including ecosystems) are closely linked and interdependent.” On January 19, we published a new four-part online series on One Health and global health security, analyzing current understanding of potential public health emergencies and exploring how effective adoption of One Health could improve global health security . Although the series focuses on pandemic preparedness, One Health goes far beyond emerging infections and new pathogens; It is the foundation for understanding and addressing the most existential threats to societies, including antimicrobial resistance, food and nutrition insecurity, and climate change.
Modern attitudes towards human health adopt a purely anthropocentric view : that the human being is the center of medical attention and concern . One Health places us in an interconnected and interdependent relationship with non-human animals and the environment . The consequences of this thought involve a subtle but quite revolutionary change in perspective: all life is equal and of equal concern . This understanding is critical to addressing pressing health issues at the human-animal-environment interface. For example, providing a growing global population with healthy diets from sustainable food systems is an urgent unmet need. It requires a complete change in our relationship with animals. The EAT-Lancet Commission takes an equitable approach by recommending people move away from an animal-based diet to a plant-based one, which not only benefits human health, but also the health and well-being of animals.
The COVID-19 pandemic provides an important example of the need for a One Health approach. Analysis of the successes and failures in managing the pandemic has prioritized health systems and the provision of vaccines and antivirals. But understanding the causes of the pandemic requires a broader ecological perspective . This lesson has not been fully learned and we therefore remain susceptible to future emerging lethal infectious diseases. The series recommends the involvement of more environmental health organizations to better integrate environmental, wildlife and agricultural issues to help address challenges related to the spread of disease.
One implication of the One Health approach is the need to reduce human pressure on the environment , an important medical intervention in itself. Take antimicrobial resistance (AMR). Driven by the use and misuse of antimicrobials in the human, animal and environmental sectors, and the spread of resistant bacteria and resistance genes within and between these sectors, antimicrobial resistance takes a huge toll globally. An estimated 1.2 million people died in 2019 from antibiotic-resistant bacterial infections with another 4.95 million deaths associated with bacterial AMR worldwide. Only by applying a One Health approach can actions to address AMR be achieved.
A major concern is the risk of worsening inequalities, as One Health networks are largely located and staffed in high-income countries. The current architecture of One Health institutions, processes, regulatory frameworks and legal instruments has given rise to a multilateral and fragmented health security landscape. A more egalitarian approach is needed, one that is not paternalistic or colonial in telling low- and middle-income countries what to do. For example, demanding that wet markets be closed to stop an emerging zoonosis might be technically correct, but failing to take into account those who make a living from those markets will only make life worse for those you claim to care about. Decolonization requires listening to what countries say and what their needs are. As the global economic crisis continues – the World Bank predicts a sharp slowdown in growth and rising debt that will hit developing countries hardest – One Health must be implemented sensitively.
The reality is that One Health will be delivered across countries, not through concordats between multilateral organisations, but by taking a fundamentally different approach to the natural world, one in which we are as concerned about the welfare of non-human animals and the environment as we are. about human beings. In its truest sense, One Health is a call for ecological equity, not just health .
Comments
The COVID-19 pandemic has exposed weaknesses in the world’s global health safety nets, says a new series of four articles published in The Lancet . The authors of the series argue that we must implement a ’One Health’ approach globally, with human, animal and environmental health organizations working together to prevent, monitor and respond to public health emergencies.
In The Lancet Series on One Health and Global Health Security , the authors call for greater investment in the One Health approach, especially for preventive and preparedness interventions for health emergencies. There is clear evidence of the benefits in terms of the number of human and animal lives saved and financial savings resulting from closer cross-sector cooperation. Billions of US dollars are required each year to have a real impact on global prevention and preparedness – a small fraction of the cost of responding to and recovering from a global health emergency like the COVID-19 pandemic.
A global analysis of One Health Networks reveals gaps and disparities in geographic distribution and partnership structures with more networks active and based in Europe and North America than other regions. The Series argues that the One Health movement must break free from power structures centered in high-income countries to establish more egalitarian global networks that address the breadth of problems and serve the communities most affected by emerging and existing threats to health. health security. Furthermore, funding priorities must move beyond subsidies and grants for an academic and development industry based in high-income countries, to focus more closely on measurable technology transfer and self-reliance in LMICs.
The series also found that environmental organizations are often not included in the design and shaping of the One Health Networks agenda, limiting the extent to which a comprehensive One Health approach is practiced. The authors call for One Health approaches to involve more community and environmental health organizations to better integrate environmental, wildlife and agricultural issues to address challenges related to disease spread and the threat of future pandemics.
Dr Osman Dar, Chatham House, London and author of the Series, says: “The COVID-19 pandemic has brought into much sharper focus the interconnectedness of human health, animal health and the state of the environment, and the catastrophic impact of underestimating the threats that arise at this interface. As countries seek to recover from the impacts of the COVID-19 pandemic, adopting integrated One Health approaches with full consideration of its underlying principles will be key to making significant progress and building back better.”
















