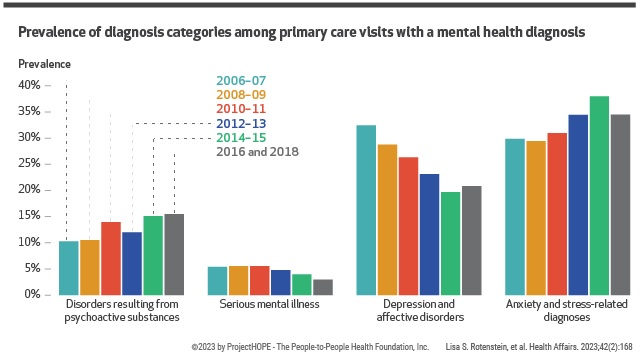
Summary A high prevalence of mental health diagnoses in adults along with the continued shortage of mental health specialists and the expansion of the patient-centered medical home have increased the involvement of primary care physicians in the treatment of mental health problems. Using nationally representative serial cross-sectional data from the 2006–18 National Ambulatory Health Care Surveys regarding visits to outpatient primary care physicians by patients eighteen years of age and older, we sought to characterize temporal trends in visits. primary care that address a mental health problem. Based on a sample of 109,898 visits representing 3,891,233,060 weighted visits, we found that the proportion of visits that addressed mental health issues increased from 10.7% of visits in 2006–07 to 15.9% in 2016 and 2018. Black patients were 40 percent less likely than White patients to have a mental health problem addressed during a primary care visit, and Hispanic patients were 40 percent less likely than non-Hispanic patients to have a mental health problem addressed during a primary care visit. These findings emphasize the need for payment and billing approaches (i.e., value-based care models and billing codes for integrated behavioral health), as well as organizational designs and supports (i.e., therapy or psychiatry providers located, availability of electronic consultations, and longer visits) that allow primary care physicians to adequately address mental health needs. |
Comments
A new study found that patients are increasingly likely to talk about their mental health problems with the doctor they often know best: their primary care doctor. Researchers at Brigham and Women’s Hospital, a founding member of the Mass General Brigham health care system, compared national data on primary care visits from 2006 and 2007 with data from 2016 and 2018, and found that the proportion of visits that addressed mental health problems increased by almost 50 percent . The team also found that African American patients and Hispanic patients were 40 percent less likely than white patients and non-Hispanic patients, respectively, to have their mental health issues addressed during their primary care visit. The results are published in Health Affairs .
"The scope of primary care has expanded and primary care physicians are more likely to provide comprehensive care, and that includes addressing mental health issues," said corresponding author Lisa Rotenstein, MD, MBA, chief medical officer of Health of Population for Brigham’s Primary Care Center of Excellence and a primary care physician in Brigham’s Division of General Internal Medicine and Primary Care. “Primary care physicians welcome the opportunity to help their patients address mental health issues, but often need better support systems to provide the care patients want and need beyond their primary care visit.”
According to 2020 data from the National Institutes of Mental Health, nearly one in five adults in the U.S. reported having a mental, emotional, or behavioral disorder. To better understand how the rise in mental health problems is affecting primary care utilization and capacity, Rotenstein and colleagues used data from the National Ambulatory Medical Care Survey (NAMCS) to compare the changes over time in the percentage of primary care visits that addressed a mental health problem.
Based on a sample of 109,898 visits , they found that the proportion of visits that addressed mental health issues increased from 10.7% of visits in 2006–07 to 15.9% in 2016 and 2018. The team also looked at a variety of factors that could change these rates, finding that there were significant differences in the likelihood of a mental health problem being addressed during a primary care visit based on the patient’s race, ethnicity, insurance type, sex, and age. patient. The team also found that mental health issues were significantly more likely to be addressed in a visit with a patient’s regular primary care doctor rather than another doctor in a practice.
“While our data doesn’t tell us why we see differences in the proportion of visits that address mental health issues when we look at rates by race and ethnicity, the findings tell us that we need to look at barriers, including process and structural disparities. and communication barriers, which can prevent all patients from accessing care as needed,” Rotenstein said.
Additionally, the authors note that the last data available for them to study was from 2018, and multiple healthcare trends and events that have emerged since that time (including the COVID-19 pandemic and increased adoption of telehealth) may have changed. the proportion of visits in primary care to address mental health problems.
“At a time when we are thinking about how primary care is delivered, our findings emphasize that the relationships we build in primary care help give our patients the opportunity to bring mental health issues to the forefront,” Rotenstein said. . “We know that mental health issues are best addressed with a team approach. Primary care can be an entry point for patients, but we must consider strategies, such as co-locating primary care providers and psychiatry providers and offering longer visits, that will allow primary care physicians to adequately address patient needs. mental health".
















