| SUMMARY |
> Background and objectives : Sex hormones can modulate the release of Calcitonin Gene Related Peptide (CGRP) in the trigeminovascular system. We studied plasma and tear fluid CGRP concentrations in female participants with episodic migraine (EM) and a regular menstrual cycle (RMC), female participants with MS and combined oral contraceptives (COC), and postmenopausal female participants with MS. For control, we analyzed three corresponding groups of age-matched female participants without MS. > Methods: CMR participants had two visits: during menstruation on day 2 ± 2 of the menstrual cycle and in the periovulatory period on day 13 ± 2. COC participants were examined on day 4 ± 2 of the hormone-free interval (HFI) and between days 7-14 of hormonal intake (HI). Postmenopausal participants were tested once at a random time. Plasma and tear fluid samples were collected at each visit to determine CGRP levels with an enzyme-linked immunosorbent assay. > Results: A total of 180 female participants (n=30 per group) completed the study. Participants with migraine and CMR showed statistically significantly higher CGRP concentrations in plasma and tear fluid during menstruation compared to participants without migraine [plasma: 5.95 pg/ml (IQR 4.37 - 10.44) vs. 4.61 pg/ml (IQR 2.83 - 6.92), p=0.020 (Mann-Whitney U test); tear fluid: 1.20 ng/ml (IQR 0.36 – 2.52) vs. 0.4 ng/ml (IQR 0.14 – 1.22), p=0.005 (Mann-Whitney U test)]. In contrast, female participants with COC and postmenopause had similar levels of CGRP in the migraine and control groups. In migraine participants with CMR, CGRP concentrations in tear fluid but not plasma during menstruation were statistically significantly higher compared to migraine participants under COC (p = 0.015 vs HFI and p = 0.029 vs HI, Mann-Whitney U test). > Discussion: Different sex hormone profiles may influence CGRP concentrations in people, with current or past ability to menstruate, with migraine. Measurement of CGRP in tear fluid was feasible and warrants further investigation. |
| Comments |
When women experience migraine attacks, it is often just before or during their menstrual period. A team of researchers from Charité – Universitätsmedizin Berlin has now identified a possible explanation. According to their study, published in the journal Neurology ,* women who experience migraines have higher levels of CGRP during menstruation. CGRP is a neurotransmitter that is known to play an important role in triggering migraines.
Women suffer migraines at three times the rate of men. Attacks tend to cluster around the time of menstruation, when they are also most severe, and the same occurs at the beginning of menopause. In many cases, symptoms improve during pregnancy and the frequency of migraines also decreases after menopause. Researchers have long known that there is a connection between hormonal fluctuations and migraines, but it is still unclear how exactly these changes trigger migraines.
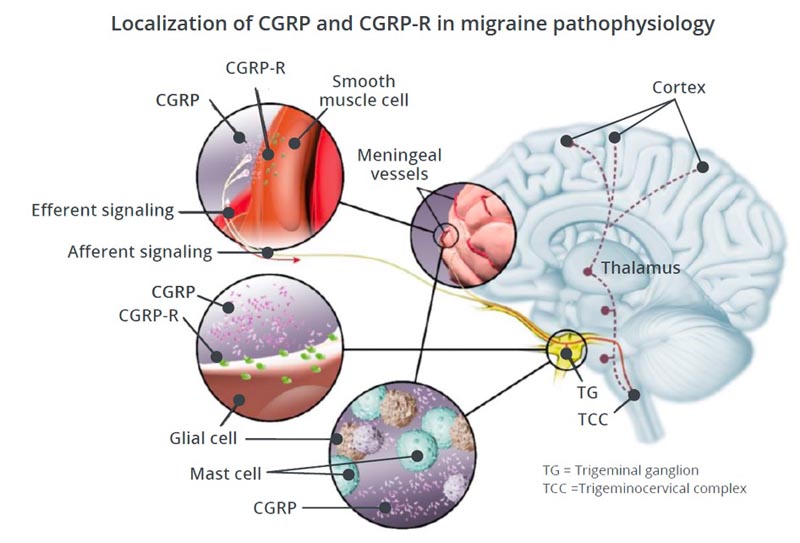
"Animal models suggest that fluctuations in female hormones, especially estrogen, lead to increased release of CGRP, an inflammatory neurotransmitter, in the brain," explains study leader Dr. Bianca Raffaelli of the Department’s Headache Center. of Neurology with Experimental Neurology at the Charité Campus in Mitte. “The full name of CGRP is calcitonin gene-related peptide .” It is a natural substance in the body, and when a person has a migraine attack, increasing levels are released, significantly dilating or widening the blood vessels in the brain. “This triggers an inflammatory response that could be one of the reasons behind the severe headaches experienced by people with migraines.”
| Increased CGRP levels during menstruation |
The Charité research group studied a total of 180 women to determine whether the link between female hormones and CGRP release also exists in humans. The researchers tested CGRP levels in migraine patients twice during their cycle, with one measurement taken during menstruation and the other during ovulation.
When the data were compared with those from women who did not suffer from migraines, it was clear that migraine patients have significantly higher concentrations of CGRP during menstruation than healthy people. “This means that when estrogen levels drop immediately before the start of a menstrual period, migraine patients release more CGRP,” says Raffaelli, who is also a member of the Clinical Scientists Program operated jointly by Charité and the Health Institute of Berlin (BIH). at Charité. "This could explain why these patients suffer more migraine attacks just before and during their monthly period."
In women taking oral contraceptives , on the other hand, there are hardly any fluctuations in estrogen levels. As the researchers demonstrated in this study, CGRP concentrations are also consistent over the course of the "artificial cycle" caused by oral contraception, with comparable levels observed in both women with migraine and healthy women. The researchers made a similar observation in postmenopausal women.
“The data will still need to be confirmed by larger studies, but our findings suggest that CGRP release depends on hormonal status in humans, as in the animal model,” says Raffaelli. “Taking birth control pills and the end of menopause actually provide relief to some migraine patients. But as our study also shows, there are women who suffer from migraines even without hormonal fluctuations. We suspect that other processes in the body play a role in triggering attacks in those patients. After all, CGRP is not the only inflammatory peptide that can cause a migraine attack.”
| Possible relevance to migraine medications |
Since CGRP plays a critical role in migraines, researchers have developed new drugs known as CGRP inhibitors to target this neurotransmitter in recent years. Raffaelli comments: “Based on our study, the question now is: do CGRP inhibitors work differently in different hormonal states? So, might it be a good idea to give these medications depending on where the person is in their cycle? More studies will be needed on these points.”
The team now plans to study what other physical processes are influenced by the menstrual cycle, which could contribute to migraine, such as the functioning of blood vessels or the excitability of the brain. The researchers also plan to take a closer look at CGRP levels in men of different age groups.
Final message In conclusion, our data suggest hormone-dependent changes in CGRP concentrations in female patients with episodic migraine. Elevated release of CGRP from the trigeminovascular system following hormonal fluctuations could help explain increased susceptibility to migraine in menstruating women. Lower tear fluid CGRP concentrations under hormonal contraception in migraine patients could be associated with altered susceptibility to migraine under hormonal therapy and should be further investigated in a longitudinal design. |
Reference : Raffaelli B et al. Sex hormones and Calcitonin Gene-Related Peptide (CGRP) in women with migraine: a cross-sectional, matched cohort study . Neurology 2023 Feb 22. doi: 10.1212/WNL.0000000000207114















