Bariatric-Metabolic Surgery Versus Lifestyle Intervention Plus Best Medical Care in Nonalcoholic Steatohepatitis (BRAVES): a Multicenter, Open-Label, Randomized Trial
Summary
Background
Observational studies suggest that bariatric-metabolic surgery could greatly improve nonalcoholic steatohepatitis (NASH). However, the effectiveness of surgery in NASH has not yet been compared with the effects of lifestyle interventions and medical therapy in a randomized trial.
Methods
We did a multicenter, open-label, randomized trial in three major hospitals in Rome, Italy. Participants aged 25 to 70 years with obesity (BMI 30 to 55 kg/m2), with or without type 2 diabetes, with histologically confirmed NASH were included. We randomly assigned (1:1:1) participants to lifestyle modification plus best medical care, Roux-en-Y gastric bypass, or sleeve gastrectomy. The primary endpoint of the study was histologic resolution of NASH without worsening fibrosis at 1-year follow-up. This study is registered with ClinicalTrials.gov, NCT03524365.
Results
Between April 15, 2019 and June 21, 2021, we biopsied 431 participants; of these, 103 (24%) did not have histological NASH and 40 (9%) refused to participate. We randomly assigned 288 (67%) participants with biopsy-proven NASH to lifestyle modification plus best medical care (n=96 [33%]), Roux-en-Y gastric bypass (n=96 [33%] ) or sleeve gastrectomy (n=96 [33%]).
In the intention-to-treat analysis, the percentage of participants meeting the primary endpoint was significantly higher in the Roux-en-Y gastric bypass group (54 [56%]) and in the sleeve gastrectomy group (55 [57%]) compared to lifestyle modification (15 [16%]; p<0·0001).
The estimated probability of resolution of NASH was 3.60 times higher (95% CI 2.19–5.92; p<0.0001) in the Roux-en-Y gastric bypass group and 3.67 times higher (2, 23 –6·02; p<0·0001) in the sleeve gastrectomy group compared to the lifestyle modification group.
In the per-protocol analysis (236 [82%] participants who completed the trial), the primary endpoint was met in 54 (70%) of 77 participants in the Roux-en-Y gastric bypass group and 55 (70%) of 79 participants in the sleeve gastrectomy group, compared with 15 (19%) of 80 in the lifestyle modification group (p<0·0001).
No deaths or life-threatening complications were reported in this study. Serious adverse events occurred in ten (6%) participants who underwent bariatric-metabolic surgery, but these participants did not require reoperations and serious adverse events resolved with medical or endoscopic treatment.
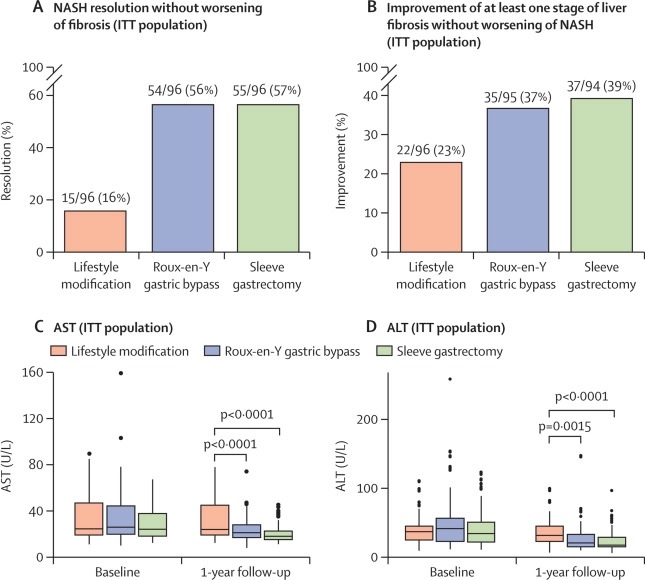
Results of primary endpoint, secondary endpoint, AST and ALT in the ITT population (A) Percentage of patients with resolution of NASH without worsening fibrosis after lifestyle modification and improved medical care, Y-gastric bypass Roux and sleeve gastrectomy in the ITT population. The data at the top of the bars are the number of responders out of the total number of individuals and the percentage of responders in each intervention group. (B) Percentage of patients with improvement of liver fibrosis in at least one stage without worsening of NASH in the lifestyle modification, Roux-en-Y gastric bypass, and sleeve gastrectomy groups in the ITT population. The data at the top of the bars are the number of responders out of the total number of individuals and the percentage of responders in each intervention group. (C) AST concentrations at baseline and 1-year follow-up in the lifestyle modification, Roux-en-Y gastric bypass, and sleeve gastrectomy groups in the ITT population. (D) ALT concentrations at baseline and 1-year follow-up in the lifestyle modification, Roux-en-Y gastric bypass, and sleeve gastrectomy groups for the ITT population. ALT=alanine aminotransferase. AST = aspartate aminotransferase. ITT=intention to treat. NASH = non-alcoholic steatohepatitis.
Interpretation
Bariatric-metabolic surgery is more effective than lifestyle interventions and optimized medical therapy in the treatment of NASH.
Money
Fondazione Policlinico Universitario A Gemelli, Policlinico Universitario Umberto I and Hospital S Camillo, Rome, Italy.
Comments
A new paper, published in The Lancet by King’s College London and the Catholic University of Rome, is the first to compare three active treatments for non-alcoholic steatohepatitis (NASH) and specifically investigate the effectiveness of metabolic surgery (blood loss surgery). weight) in a randomized clinical trial.
Nonalcoholic fatty liver disease (NAFLD) is the most common cause of chronic liver disease, affecting 55% of people with type 2 diabetes and 75% of people with obesity globally. Non-alcoholic steatohepatitis (NASH) is the progressive form of the disease and is characterized by injury and inflammation of liver cells, which induce liver fibrosis (tissue scarring). If left untreated, it can lead to liver failure and liver cancer, and is one of the leading causes of liver transplantation in the Western world. NASH also increases the risk of cardiovascular disease and overall mortality in patients with obesity or type 2 diabetes. NAFLD/NASH currently affects 12% of adults in the UK; In the US, the condition is estimated to affect 27 million people by 2030.
The multicenter randomized trial was conducted in Italy. The trial compared the effectiveness of bariatric and metabolic surgery against lifestyle modifications and current best medical care in 288 patients.
Pre- and postoperative liver biopsies showed that surgery was most effective in inducing complete reversal of inflammation and cellular damage in the liver, the central features of NASH, without worsening liver fibrosis after 1 year of surgery. The likelihood of achieving NASH reversal was 3 to 5 times higher with metabolic surgery than with medical care. Surgery was also more effective in achieving improvement in at least one stage of liver fibrosis, another predetermined endpoint of the trial. The two surgical procedures appeared to improve NASH equally.
The researchers say that the ability of surgery to control and even improve fibrosis associated with NASH has special clinical relevance, since fibrosis is the main predictor of liver complications and poor cardiovascular outcomes and death in patients with NASH.
Professor Geltrude Mingrone, first author of the report, Professor of Medicine at the Catholic University of Rome and Professor of Diabetes and Nutrition at King’s College London, said: "The results of our study support the use of metabolic surgery as a treatment for NASH, a condition long considered orphan of effective therapies.”
Professor Francesco Rubino, Senior Co-Investigator and Chair of Metabolic and Bariatric Surgery at King’s College London and Consultant Surgeon at King’s College Hospital, said: "The presence of NASH predicts a significant risk of complications and mortality in people with severe and type 2 obesity. diabetes. The results of this study provide a compelling case for prioritizing metabolic surgery in this patient population."
Compared to conventional medical treatment, surgery also resulted in better overall health benefits. Although both surgical procedures appeared to equally improve NASH, the gastric bypass group was more effective than sleeve gastrectomy in improving type 2 diabetes and reducing other cardiovascular risk factors associated with NAFLD/NASH.
Added value of this study To our knowledge, BRAVES is the first randomized trial to compare the effects of bariatric-metabolic surgery with lifestyle modification plus best medical care in people with histologically confirmed NASH. Surgical treatment resulted in resolution of NASH without worsening fibrosis according to the pathologist’s diagnostic evaluation and the nonalcoholic fatty liver disease activity scoring algorithm proposed by the NASH Clinical Research Network. Per-protocol analysis showed that this goal was achieved in 70% of patients who underwent Roux-en-Y gastric bypass or sleeve gastrectomy, far exceeding the effects of any drug tested so far in randomized trials. . Importantly, the more severe the NASH and liver fibrosis, the higher the proportion of patients with NASH resolution. The improvement of at least one stage of fibrosis severity without worsening of NASH was almost twice that of the control group. Implications of all available evidence In participants with a nonalcoholic fatty liver disease activity score of at least 4 and stage 2 or 3 fibrosis, the likelihood of resolution of NASH without worsening fibrosis was 4·40 times greater in the bypass group Roux-en-Y gastric and 3·43 times higher in the sleeve gastrectomy group than in the lifestyle modification group. In this subgroup, the improvement of at least one stage of fibrosis was almost twice as high after Roux-en-Y gastric bypass and sleeve gastrectomy than after lifestyle modification. The ability of surgery to control and even improve fibrosis associated with NASH has special clinical relevance given that fibrosis is the main predictor of liver complications and cardiovascular morbidity and mortality in NASH. These findings further support the use of bariatric-metabolic surgery in people with metabolic diseases. NASH should be considered as an important factor in making decisions about prioritizing surgery in people with obesity and type 2 diabetes. |
















