Decompressive craniectomy is a surgical procedure in which a large section of the skull is removed and the underlying dura mater is widely opened. The procedure has been shown to reduce mortality when used as a last-level treatment for post-traumatic intracranial hypertension but is associated with an increased risk of unfavorable outcomes when used as a second-level treatment. However, the most common indication for a decompressive craniectomy is a traumatic subdural hematoma.
Because acute subdural hematomas are often associated with underlying parenchymal brain injury, intraoperative or postoperative brain swelling may be encountered. Therefore, a primary decompressive craniectomy is often performed at the time of evacuation of an acute subdural hematoma, either due to inflammation of the brain that does not allow replacement of the bone flap without compressing the brain or preemptively in anticipation of inflammation. in the following days according to clinical judgment. In the first situation, the bone flap must be left outside. However, there is limited evidence regarding the added value of performing decompressive craniectomy preventively in this setting.
The effectiveness of a primary decompressive craniectomy (no bone flap) compared with a craniotomy (bone flap replacement) for the evacuation of acute subdural hematomas has not been adequately studied. It is important to address this choice in a trial, particularly because craniectomy requires a subsequent operation to reconstruct the skull (called cranioplasty) which has risks. We conducted a multicenter, randomized, controlled trial to compare the outcomes of craniotomy and decompressive craniotomy in adult patients with traumatic acute subdural hematoma.
Background
Traumatic acute subdural hematomas frequently warrant surgical evacuation via craniotomy ( bone flap replacement) or decompressive craniectomy (without bone flap replacement). Craniectomy may prevent intracranial hypertension, but it is unclear whether it is associated with better outcomes.
Methods
We conducted a trial in which patients undergoing surgery for traumatic acute subdural hematoma were randomly assigned to undergo craniotomy or decompressive craniectomy . An inclusion criterion was a bone flap with an anteroposterior diameter of 11 cm or more.
The primary outcome was the Glasgow Outcome Scale Extended (GOSE) score (an 8-point scale, ranging from death to “good recovery” [no injury-related problems]) at 12 months.
Secondary outcomes included GOSE score at 6 months and quality of life assessed by the EuroQol Group 5-Dimension 5-Level (EQ-5D-5L) questionnaire.
Results
A total of 228 patients were assigned to the craniotomy group and 222 to the decompressive craniectomy group. The median bone flap diameter was 13 cm (interquartile range, 12 to 14) in both groups.
The common odds ratio for differences between GOSE scores at 12 months was 0.85 (95% confidence interval, 0.60 to 1.18; P = 0.32). The results were similar at 6 months.
At 12 months, death had occurred in 30.2% of patients in the craniotomy group and 32.2% of those in the craniotomy group; A vegetative state was present in 2.3% and 2.8%, respectively, and good recovery, minor or major, in 25.6% and 19.9%.
EQ-5D-5L scores were similar in the two groups at 12 months. Additional cranial surgery was performed within 2 weeks of randomization in 14.6% of the craniotomy group and 6.9% of the craniectomy group.
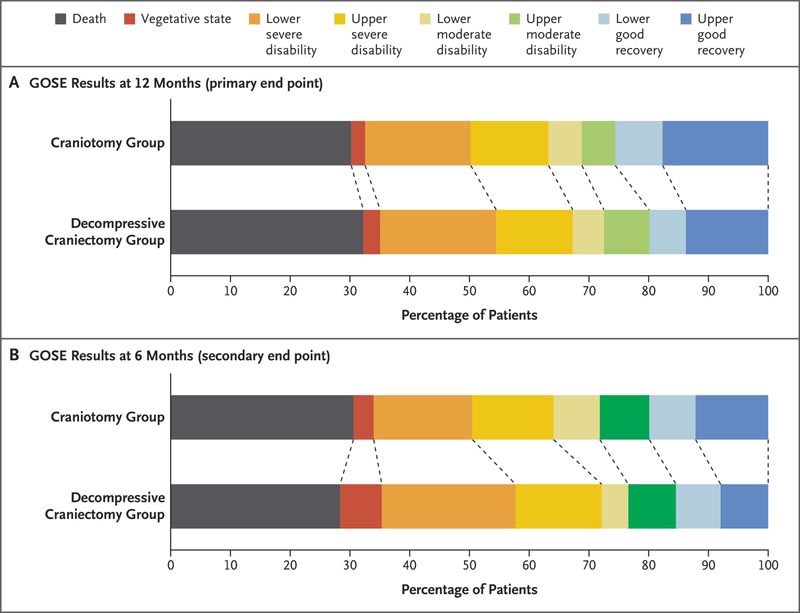
Figure : Glasgow Outcome Scale Extended (GOSE) results at 6 and 12 months.
Conclusions Among patients with traumatic acute subdural hematoma who underwent craniotomy or decompressive craniectomy, disability and quality of life outcomes were similar with the two approaches. Additional surgery was performed in a greater proportion of the craniotomy group, but more wound complications occurred in the craniotomy group. |
Discussion
In this trial involving adult patients with traumatic acute subdural hematomas warranting surgical evacuation, we found no significant differences in GOSE results between the craniotomy (bone flap replacement) group and the decompressive craniectomy (bone flap replacement) group. ) at 12 months, and results for most secondary outcomes were similar in the two groups.
Uniformly accepted criteria are lacking to predict the development of postoperative brain swelling and elevated intracranial pressure in this setting and to inform the choice of craniotomy or decompressive craniectomy for hematoma evacuation. Systematic literature reviews have not identified randomized trials that address the issue that led to this trial; In non-randomized studies, conclusions have been limited due to confounding by indication. Therefore, the role of a preventive decompressive craniectomy in this setting is not known and has been identified as a research priority.
Although the present trial showed no significant difference in mortality or GOSE outcomes between the craniotomy group and the decompressive craniectomy group, additional cranial operations within 2 weeks of randomization were performed more frequently in the decompressive craniectomy group. craniotomy and most of them were decompressive craniectomies for brain inflammation. However, patients in the decompressive craniectomy group had more wound-related complications and surgical site infections . Although disability and other outcomes were similar in the two groups, the trial may have practical implications. If the bone flap can be replaced without compressing the brain, surgeons may consider doing so, rather than performing a preemptive decompressive craniectomy. These findings may not be relevant to military or resource-limited settings.
In this trial involving adult patients undergoing evacuation of a traumatic acute subdural hematoma, decompressive craniectomy and craniotomy yielded similar results with respect to overall outcomes at 12 months. Additional craniectomies were performed more frequently in the craniotomy group, but wound complications and surgical site infections occurred more frequently in the decompressive craniectomy group.
(Funded by the National Institute for Health and Care Research; RESCUE-ASDH ISRCTN registration number, ISRCTN87370545. opens in new tab.)
















