Clinical vignette A 25-year-old man is brought to the emergency department by EMS after sudden-onset right testicular pain while playing basketball. He denies trauma or contact to the scrotum or perineum; however, he endorses sudden, severe pain associated with nausea and nonbloody, nonbilious emesis. Additionally, he complains of mild tenderness in his right lower abdomen. Otherwise, the systems review is nothing special. Vital signs include:
On examination, he appears uncomfortable and does not have a tender abdomen. He has a normal penile examination, but the right hemiscrotum has mild erythema, a horizontal position, and is exquisitely tender. |
Question : What is the next step in your evaluation and diagnosis?
Answer : Testicular torsion
Epidemiology
- Bimodal incidence: 1st year of life and adolescence (12-18 years).
- Rare case reports of men aged > 40 years with cases of testicular torsion.
- 50% of patients with testicular torsion have a previous episode of torsion that resolved spontaneously.
- Testicular pain accounts for 1% of emergency department visits annually.
Anatomy
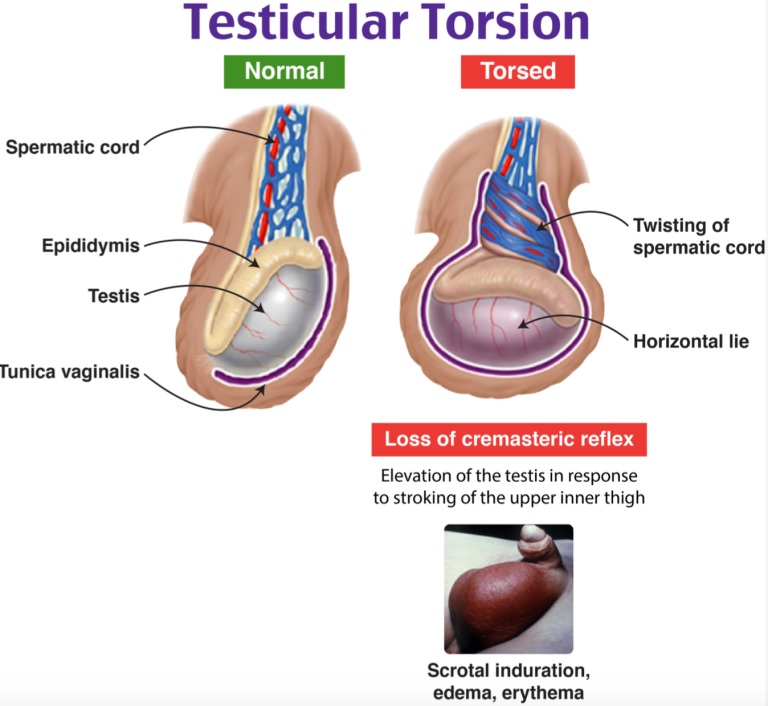
Testicular torsion is caused by twisting of the testicle in its blood supply, occluding the vascular pedicle, leading to vascular congestion and testicular ischemia.
The tunica vaginalis is attached to the scrotal wall on the posterolateral side, preventing movement of the testicles within the scrotum.
If this union occurs too superiorly, known as clapper deformity , it allows torsion of the testicle.
Clinical presentation:
Signs and symptoms:
Symptoms : acute unilateral testicular pain, nausea, vomiting, abdominal pain.
Signs : absent cremasteric reflex, swelling, testicular tenderness, abnormal testicular position, palpable spermatic cord knot.
20% of testicular torsion will present with isolated abdominal pain without testicular pain.
The sensitivity of the cremasteric reflex in testicular torsion varies, reaching up to 60%.
Testicular position is often difficult to determine, although if there is an elevated testicle, OR= 58.8.
The cremasteric reflex is not present in a significant portion of patients at baseline and may be present in those with torsion.
Study of n=120, 91% of patients with confirmed torsion had a positive Prehn sign and 21% of those diagnosed with epididymitis had a positive Prehn sign.
Differential diagnosis : Epididymitis, torsion of the testicular appendix, varicocele, spermatocele, testicular rupture, appendicitis, nephrolithiasis, ureterolithiasis, AAA, intestinal obstruction, mesenteric adenitis.
Assessment:
Evaluate ABC
+/- low-grade fever, late stage may have hypotension and tachycardia due to tissue necrosis, although this is less common.
Perform a complete physical examination
Abdomen : Right or left lower quadrant tenderness due to referred pain, although the abdomen may not be peritoneal.
Genito-urinary : Erythema, edema, horizontal position, high testicle, negative cremasteric reflex is classic.
Clinical decision tool :
Testicular evaluation for ischemia and suspected torsion ( TWIST ).
- Presence of testicular inflammation: 2 points
- Presence of hard testicle: 2 points
- Absence of cremasteric reflex: 1 point
- Presence of high testicle: 1 point
- Presence of nausea/vomiting: 1 point
High risk : 6-7 points, without images, suggests that immediate urological detorsion is needed
PPV 100% when >7 pts
Intermediate risk : 1-5 points, obtain ultrasound, consider differential diagnosis.
NPV 96% when < 5 points
Low risk : 0 points even if clinical suspicion is maintained with an incredibly low threshold for ordering an ultrasound.
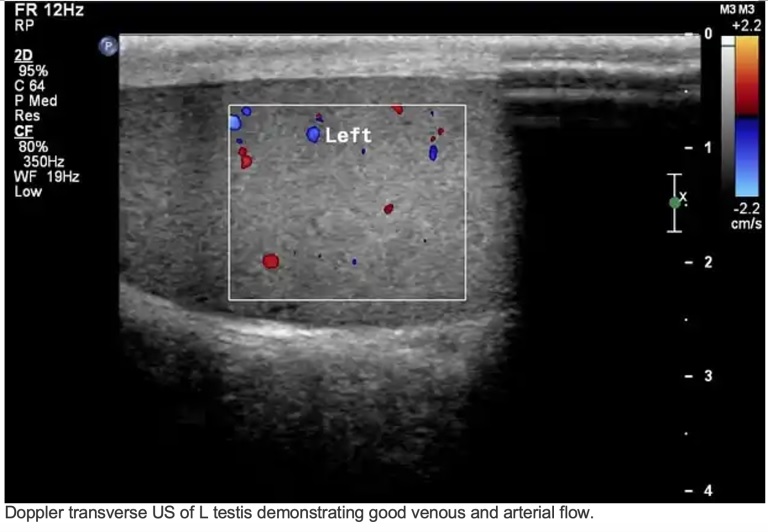
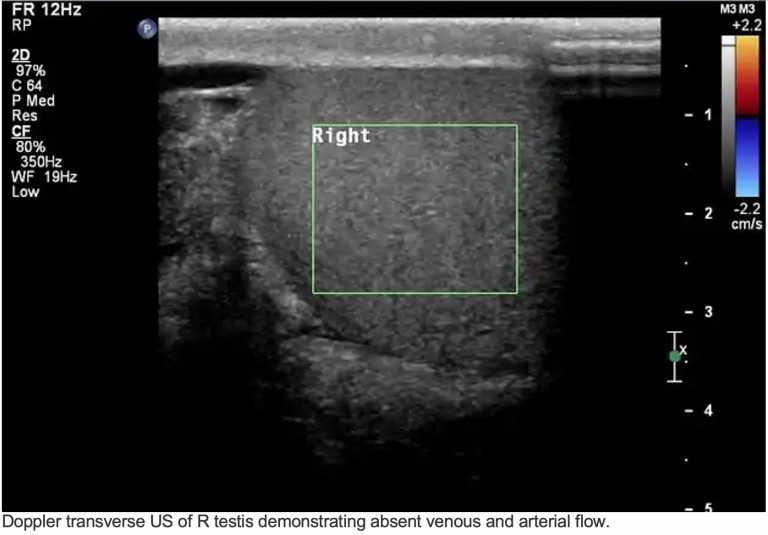
Images:
Doppler ultrasound
- Sensitivity 88-100% (+LR 8.8-10)
- Specificity 90%
High-resolution ultrasound improves sensitivity and specificity to 96 and 99%, respectively.
Ultrasound functions :
Decreased Doppler flow compared to unaffected contralateral testes
Note: Subject to false negatives with arterial but not venous flow or abnormally high resistance arterial flow.
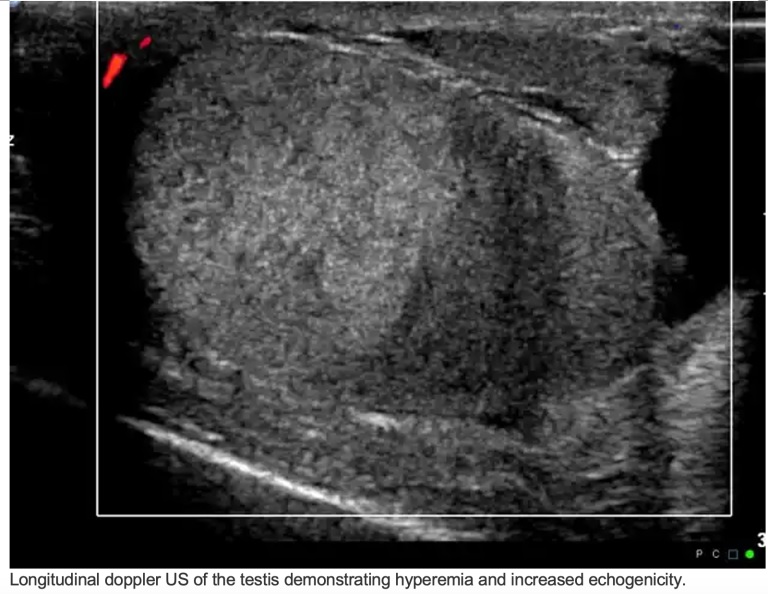
Greater echogenicity
Enlarged hyperemic testis
Swirl sign: spiral-shaped pattern of the spermatic cord
Magnetic resonance imaging (MRI): not recommended for urgent testicular pathology since the time until detorsion is key.
- Sensitivity 93%
- 100% specificity
Laboratory evaluation:
Usual routine and coagulogram
Consider testing for sexually transmitted infections
Treatment:
- Pain control and IV rehydration.
- Urology consultation due to detorsion and bilateral orchiopexy.
- 40% of patients will have bell clapper deformity on the contralateral side.
- Detorsion within 4 hours yields a 96% successful rescue.
- Salvage rates decrease to 10% when delayed more than 24 hours.
- If there is a significant delay in detorsion, consider a manual detorsion of 540 degrees.
- Medial to lateral detorsion is recommended; however, this is unsuccessful in 1/3 of patients, who may twist in the opposite direction.
- Sedation and analgesia are recommended, but medication must be administered judiciously to preserve mental status to evaluate successful detorsion.
- Evaluate with ultrasound after attempted detorsion.
- The patient still requires urologic evaluation in the operating room and orchidopexy after successful detorsion in the ED.
Note : Manual detorsion is appropriate only when emergency surgical care is not available, as manual attempts can worsen the torsion when rotated laterally, which occurs one-third of the time. When manual detorsion is attempted, it should be medial to lateral manual detorsion, not lateral to medial.
A scrotal ultrasound is the recommended first-line imaging test to rule out or confirm testicular torsion and should only be performed before surgical consultation when patients with testicular pain have reassuring findings on history and examination.
Urine studies are useful in ruling out sexually transmitted epididymitis or a urinary tract infection, but rarely present with testicular pain.
Highlights
|
Score Twist : Frohlich LC, et al. Prospective Validation of Clinical Score for Males Presenting with an Acute Scrotum. Acad Emerg Med . 2017 Dec;24(12):1474-1482.















