Research Highlights:
|
Summary
Subclinical cardiovascular disease in US adults with and without diabetes
Background
We characterized the burden and prognostic value of subclinical cardiovascular disease (CVD) assessed by cardiac biomarkers among adults with and without diabetes in the general US population.
Methods and Results
We measured hs‐cTnT (high‐sensitivity cardiac troponin T) and NT‐proBNP (N‐terminal B‐type natriuretic peptide) in stored serum samples from the National Health and Nutrition Examination Survey from 1999 to 2004. Among adults from USA without a history of CVD (n = 10,304), we estimated the prevalence of elevated hs‐cTnT (≥14 ng/L) and NT‐proBNP (≥125 pg/mL) in those with and without diabetes.
We examined associations between elevated hs‐cTnT and NT‐proBNP with all‐cause and CVD mortality after adjustment for demographics and traditional CVD risk factors. The crude prevalence of subclinical CVD (elevated hs‐cTnT or NT‐proBNP) was ≈2‐fold higher in adults with (vs. without) diabetes (33.4% vs. 16.1%).
After adjustment for age, elevated hs‐cTnT, but not elevated NT‐proBNP, was more common in patients with diabetes, overall and by age, sex, race and ethnicity, and health status. weight. The prevalence of elevated hs‐cTnT was significantly higher in those with longer duration of diabetes and worse glycemic control.
In people with diabetes, elevated hs-cTnT and NT-proBNP were independently associated with all-cause mortality (adjusted hazard ratio [HR], 1.77 [95% CI, 1.33– 2.34] and HR, 1.78 [95% CI, 1.26–2.51]) and CVD mortality (adjusted HR, 1.54 [95% CI, 0.83–2.85] and HR , 2.46 [95% CI, 1.31–4.60]).
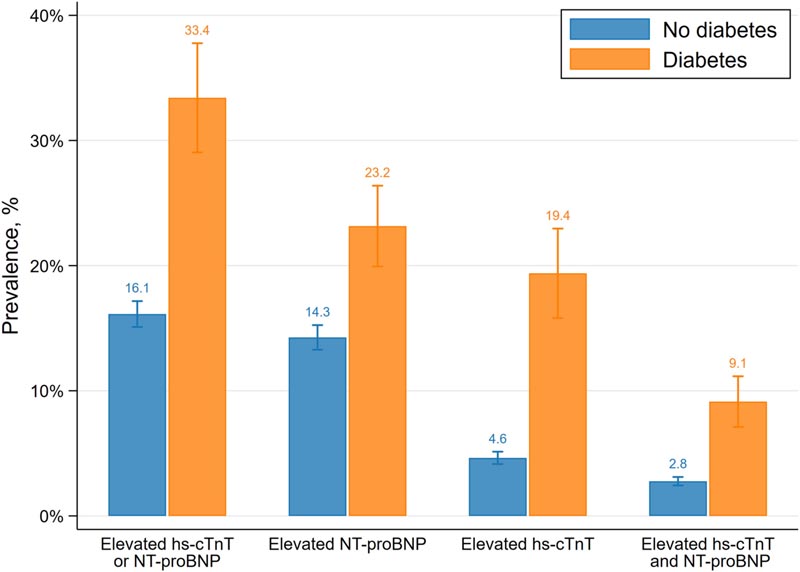
Figure . Crude prevalence of subclinical cardiovascular disease in asymptomatic US adults by diabetes status (National Health and Nutrition Examination Survey 1999–2004).
Conclusions
Subclinical CVD affects ≈1 in 3 US adults with diabetes and confers a substantial risk of mortality. Routine cardiac biomarker testing may be useful in assessing and monitoring risk in people with diabetes.
Comments
1 in 3 adults with type 2 diabetes may have undetected cardiovascular disease.
Elevated levels of two protein biomarkers that indicate heart damage were associated with undetected or asymptomatic cardiovascular disease in adults with type 2 diabetes compared to those without type 2 diabetes, according to new research published in the Journal of the American Heart Association . an open access, peer-reviewed journal of the American Heart Association .
Tests for high-sensitivity cardiac troponin T and N-terminal B-type natriuretic peptide biomarkers are used to measure injury and stress in the heart. These tests are routinely used to diagnose heart attacks and heart failure. However, slightly elevated concentrations of these proteins in the bloodstream may be an early warning sign of changes in the structure and function of the heart, which may increase the risk of heart failure, coronary heart disease, or death in the future.
"What we’re seeing is that many people with type 2 diabetes who have not had a heart attack or history of cardiovascular disease are at high risk for cardiovascular complications," said study co-author Elizabeth Selvin, Ph.D., MPH, professor of epidemiology at the Johns Hopkins Bloomberg School of Public Health in Baltimore. “When we look at the entire population of people diagnosed with type 2 diabetes, about 27 million adults in the US, according to the CDC, some are at low risk and some at high risk for cardiovascular disease, so the open question is “Who is most at risk?” These cardiac biomarkers give us a window into cardiovascular risk in people who would not otherwise be recognized as being at higher risk.”
Researchers analyzed health information and blood samples from more than 10,300 adults collected as part of the U.S. National Health and Nutrition Examination Survey from 1999 to 2004. The goal was to determine whether cardiovascular disease without previously symptoms recognized could be determined by elevated levels of cardiac protein biomarkers between people with and without type 2 diabetes. Study participants reported no history of cardiovascular disease when they enrolled in the study.
Using stored blood samples from all study participants, the researchers measured the levels of two cardiac biomarkers. Mortality statistics were collected from the National Death Index. After adjusting for age, race, income, and cardiovascular risk factors, they evaluated associations between elevated troponin and N-terminal pro B-type natriuretic peptide with risk of death from cardiovascular or all-cause death.
The study found:
|
“Cholesterol is often the factor we target to reduce the risk of cardiovascular disease in people with type 2 diabetes. However, type 2 diabetes can have a direct effect on the heart unrelated to cholesterol level . "If type 2 diabetes is causing direct damage to the small vessels of the heart unrelated to cholesterol plaque buildup, then cholesterol-lowering medications are not going to prevent heart damage," Selvin said. "Our research suggests that additional non-statin therapies are needed to reduce the risk of cardiovascular disease in people with type 2 diabetes."
Much of the research has focused on studying how traditional risk factors, such as high blood pressure and cholesterol, affect cardiovascular health; However, emerging evidence suggests that screening for certain cardiac biomarkers should be added to routine evaluation of traditional cardiovascular risk factors.
“The biomarkers analyzed in this study are very powerful to systematically categorize patients according to their health status. “Measuring biomarkers more routinely can help us focus on cardiovascular prevention therapies for people with type 2 diabetes who are at higher risk,” she added.
This is one of the first studies to use participants who truly reflect the general population. However, since the data did not allow for the identification of heart disease, heart failure, stroke, or cardiovascular complications, further research is needed to determine whether routine measurement of these biomarkers can reduce cardiovascular complications in this population.
According to the American Heart Association’s 2023 Statistical Update, 102,188 deaths in the US in 2020 were attributed to diabetes (including type 1 and type 2 diabetes) and an estimated 1.64 million deaths worldwide. the world.
In conclusion , subclinical CVD poses a significant public health challenge for adults with diabetes. Approximately 1 in 3 adults with diabetes have subclinical CVD as assessed by cardiac biomarkers, with higher rates in people with long-standing diabetes or poor glycemic control. Subclinical CVD was independently associated with an increased risk of mortality. Routine testing of cardiac biomarkers may be useful to assess and monitor cardiovascular risk in people with diabetes in the general population.
Clinical Perspective What’s new? We measured cardiac biomarkers (high-sensitivity cardiac troponin and terminal BN-type natriuretic peptide) in a nationally representative sample of US adults with and without diabetes. Approximately 1 in 3 adults with diabetes had evidence of subclinical cardiovascular disease assessed by cardiac biomarkers. Subclinical cardiovascular disease was strongly associated with increased risk of mortality in adults with diabetes, even after adjusting for demographic characteristics and cardiovascular risk factors. What are the clinical implications? The substantial burden of subclinical cardiovascular disease in adults with diabetes highlights the urgent need for prevention. Cardiac biomarkers may be useful for assessing and monitoring risk in people with diabetes in the general population. |
Co-authors are Michael Fang, Ph.D., MHS; Dan Wang, M.S.; Olive Tang, M.D., Ph.D., M.H.S.; John William McEvoy, M.B., B.Ch., BAO, M.H.S., M.Ed., Ph.D.; Justin B. Echouffo-Tcheugui, M.D., Ph.D.; and Robert H. Christenson, Ph.D. Author disclosures are listed in the manuscript.
The study was funded by the Biomarkers Consortium of the Foundation for the National Institutes of Health.
















