PCI or CABG for Left Main Coronary Artery Disease: The SWEDEHEART Registry
Goals
A Nationwide Prospective All-Attendee Observational Registry Study to Analyze Outcomes After Coronary Artery Bypass Grafting (CABG) or Percutaneous Coronary Intervention (PCI) in Left Main Coronary Artery (LMCA) Disease Without protection.
Methods and results
All patients undergoing coronary angiography in Sweden are registered in the Swedish web system for the improvement and development of evidence-based care in cardiac diseases evaluated according to the registry of recommended therapies.
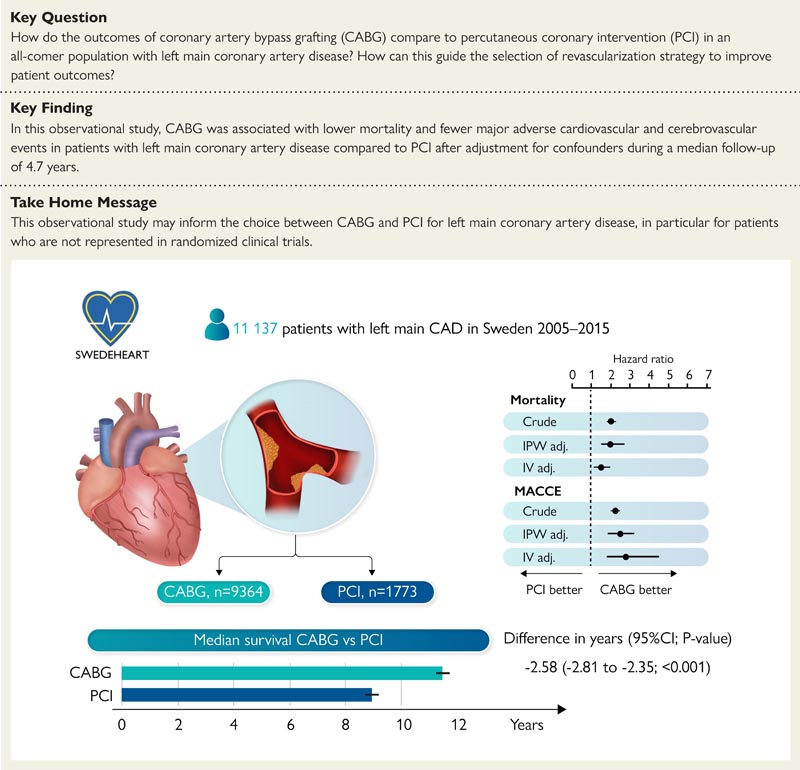
Between 01/01/2005 and 12/31/2015, 11,137 patients with LMCA disease underwent CABG (n = 9,364) or PCI (n = 1,773). Patients with prior CABG, ST-segment elevation myocardial infarction (MI), or cardiac shock were excluded .
Death, myocardial infarction, stroke, and repeat revascularization during follow-up through 12/31/2015 were identified through national registries. Cox regression was used with inverse probability weighting (IPW) and an instrumental variable (IV), administrative region.
Patients undergoing PCI were older, had a higher prevalence of comorbidities but a lower prevalence of three-vessel disease.
PCI patients had higher mortality than CABG patients after adjustment for known cofounders with IPW analysis (hazard ratio [HR] 2.0 [95% confidence interval (CI) 1.5–2, 7]) and known/unknown confounders with IV analysis (HR 1.5 [95% CI 1.1–2.0]).
PCI was associated with a higher incidence of major adverse cardiovascular and cerebrovascular events (MACCE; death, MI, stroke, or repeat revascularization) than CABG, with analysis IV (HR 2.8 [95% CI 1.8-4, 5]).
There was a quantitative interaction for diabetic status with respect to mortality (P = 0.014), resulting in 3.6 years (95% CI: 3.3–4.0) longer median survival time favoring CABG in patients with diabetes .
Conclusion In this nonrandomized study, CABG in patients with LMCA disease was associated with lower mortality and less MACCE compared with PCI after multivariable adjustment for known and unknown confounders. |
















