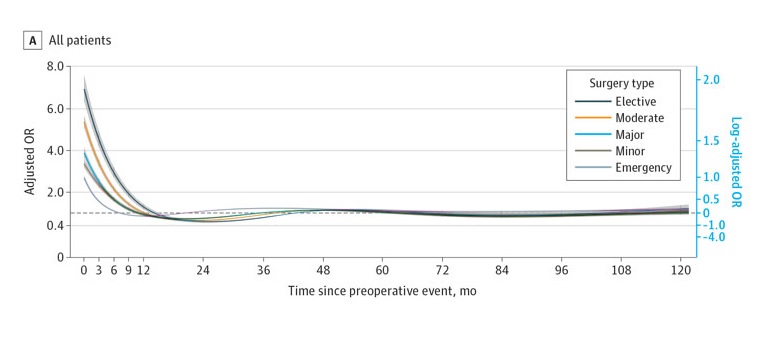
Key points Is time since a cardiovascular event associated with an increased risk of mortality in patients undergoing non-neurological or non-cardiac surgery? Findings In this study, the increased risk of postoperative mortality after elective surgery decreased with time since the cardiovascular event, with a plateau approximately 14 months after the event. A similar pattern was seen with emergency surgery, but plateaued shortly after the event. Meaning The findings indicate that physicians must weigh the potential benefits of surgery against the risk of increased mortality from too rapid surgery after a recent cardiovascular event. |
Importance
There is a lack of consensus regarding the risk range for time-dependent postoperative mortality after acute coronary syndrome or stroke.
Aim
To determine the magnitude and duration of risk associated with the time interval between a preoperative cardiovascular event and 30-day postoperative mortality.
Design, environment and participants
This is a longitudinal retrospective population-based cohort study. This study linked data from NHS England’s Hospital Episode Statistics, the National Myocardial Ischemia Audit Project and the Office for National Statistics mortality register.
We included all adults undergoing NHS-funded non-cardiac and non-neurological surgery in England between 1 April 2007 and 31 March 2018, recorded in Admitted Care Hospital Episode Statistics. . Data was analyzed from July 2021 to July 2022.
Exposure
The time interval between a previous cardiovascular event (acute coronary syndrome or stroke) and surgery.
Main results and measures
The primary outcome was 30-day all-cause mortality .
Secondary outcomes were postoperative mortality at 60, 90, and 365 days. Multivariable logistic regression models with restricted cubic splines were used to estimate adjusted odds ratios.
Results
There were 877,430 patients with and 20,582,717 without a prior cardiovascular event (overall mean [SD] age, 53.4 [19.4] years; 11,577,157 [54%] women).
Among patients with a prior cardiovascular event, the time interval associated with an increased risk of postoperative mortality was surgery within 11.3 months (95% CI, 10.8-11.7), with subgroup risks 14.2 months before elective surgery (95% CI, 13.3-15.3) and 7.3 months for emergency surgery (95% CI, 6.8-7.8).
Heterogeneity in these times was observed in many surgical specialties. The time-dependent risk intervals after stroke and myocardial infarction were similar, but the absolute risk was higher after stroke.
Regarding surgical urgency, the risk of 30-day mortality was higher in those with a previous cardiovascular event for emergency surgery (adjusted hazard ratio, 1.35; 95% CI, 1.34-1.37) and an elective procedure (adjusted hazard ratio, 1.83; 95% CI, 1.78-1.89) than those without a prior cardiovascular event.
Conclusions and relevance In this study, surgery within the first year of acute coronary syndrome or stroke was associated with increased postoperative mortality before reaching a new baseline, particularly for elective surgery. This information may help physicians and patients balance deferring the potential benefits of surgery with the desire to avoid increased mortality from too-rapid surgery after a recent cardiovascular event. |
















