Thousands of controlled trials support the effectiveness of psychological therapy and antidepressant medication in treating emotional disorders. The combination of psychotherapy and antidepressants improves therapeutic response, suggesting complementary proximal mechanisms .
Influential neural theories conceptualize psychotherapy as directed affect circuitry through prefrontal cortical mechanisms, and antidepressants as altering affect processing directly through effects on subcortical structures such as the amygdala.
There is substantial evidence that both psychotherapy and antidepressant medication alter emotion and reward processing, thereby normalizing affective processing.
However, they are believed to change affective processing through different (different) cognitive routes. For example, psychotherapy can change the cognitive control of affect processing or attention and awareness of the affective state, while antidepressants can alter the generation of affective and visceral sensations.
The different proximal mechanisms of psychotherapy and antidepressants could explain the different outcomes of these treatments, including the particular advantage of psychotherapy compared to antidepressants in preventing relapse. Evidence of different cognitive mechanisms would be supported by different neural changes after antidepressant medication and psychotherapy; Evidence against this theory would be supported if the two treatments only evoked overlapping changes.
Theories of different proximal mechanisms have now been tested using neuroimaging (such as functional magnetic resonance imaging) to measure brain activation before and after a typical course of antidepressants or psychotherapy. Some empirical work supports differential mechanisms.
Several studies show changes in activation in the amygdala, hippocampus , or other subcortical regions as a result of antidepressant medication, while changes in prefrontal cortex regions are commonly reported after psychotherapy. However, when the two are directly contrasted, distinct mechanisms are not always found.
Neuroimaging meta-analysis is a statistically powerful and generalizable approach to elucidate whether neural changes from psychotherapy and antidepressant medication reliably diverge or converge.
Using primary data from two meta-analyses, we tested whether treatment with antidepressants or psychotherapy evoked overlapping or distinct neural changes. We then separately tested whether neural changes from antidepressant medication or psychotherapy overlapped with known affective circuits, using data from a third meta-analysis of affective processing in the brain.
Consistent with influential theoretical models, we anticipated that both psychotherapy and antidepressants would evoke changes in the affective network, but that psychotherapy would change the prefrontal regions involved in attention and awareness of affect processing while antidepressants would change the subcortical regions involved. in the generation of affective and visceral sensations.
Background
Influential theories predict that antidepressant medication and psychological therapies evoke distinct neural changes.
Goals
Test the convergence and divergence of neuronal changes caused by antidepressants and psychotherapy, and their overlap with the brain’s affective network.
Method
We employed a quantitative synthesis of three meta-analyses (n = 4206). First, we assessed common and distinct neural changes elicited by antidepressant medication and psychotherapy, contrasting two comparable meta-analyses reporting the neural effects of these treatments.
Both meta-analyses included patients with affective disorders, including major depressive disorder, generalized anxiety disorder, and panic disorder. Most were evaluated using negatively valenced tasks during neuroimaging.
Next, we assessed whether neural changes caused by antidepressants and psychotherapy overlapped with the brain’s affective network, using data from a third meta-analysis of affect-based neural activation.
Results
Neural changes from psychotherapy and antidepressant medication did not converge significantly in any region.
Antidepressants evoked neural changes in the amygdala , while psychotherapy evoked anatomically distinct changes in the medial prefrontal cortex .
Both psychotherapy- and antidepressant-related changes converged separately across regions of the affective network .
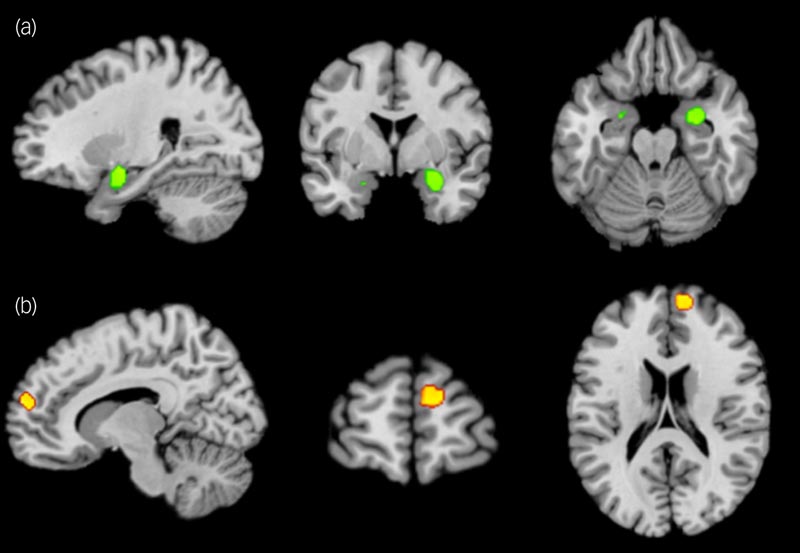
Neural changes after antidepressant treatment versus psychological therapy for affective disorders. (a) Preferential involvement of the bilateral amygdala and right medial globus pallidus in antidepressant treatment versus psychotherapy. (b) Preferential involvement of the medial prefrontal cortex in psychotherapy versus antidepressant treatment. No convergence of changes was found. All results were thresholded at P < 0.05 cluster-corrected family error (initial cluster formation threshold P < 0.001). For visualization, Z maps were overlaid on a standard brain in MNI space (Colin27, a stereotaxic average of 27 anatomical scans from a single subject, with the skull stripped) using Mango software.
Conclusions This supports the notion of specific brain effects of antidepressant treatment and psychotherapy. Both treatments induce changes in the affective network, but our results suggest that their effects on affect processing occur through different proximal neurocognitive mechanisms of action. |
Discussion
We demonstrate treatment- specific brain effects following antidepressant treatment versus psychotherapy, consistent with theories of different proximal mechanisms of action. However, the effects of both interventions overlap with a network involved in the representation of affective states.
Psychotherapy is believed to target cognitive processes and ’negative schemas’ through prefrontal control over the processing of affective information mediated by the limbic system. In the context of our findings, psychotherapy could alter attention and awareness of the affective state through changes in mPFC function.
In contrast, antidepressants could target the affective or visceromotor state of the brain directly by altering the brain’s limbic structures involved in generating a negative affective bias. An example of these brain structures is the amygdala , the central site of the results of our antidepressants. Changes in the amygdala after treatment with antidepressants (predominantly SSRIs) could have resulted from increased availability of serotonin at synapses, leading to inhibition of the amygdala .
We show that the divergent effects of psychotherapy and antidepressant medication overlap, however, with the brain’s affective network.
This overlap could explain the improved efficacy of combined pharmacological and psychological treatment. The dorsomedial prefrontal cortex and amygdala are reliably engaged during affective (versus neutral) processing; however, they can participate in functionally dissociable processes.
Previous work suggests that the dorsomedial prefrontal node is involved in focusing conscious attention on feelings and that the amygdala is involved in driving changes in affective fluctuations.
Psychotherapy and antidepressants also appear to differentially target these psychological processes, which may contribute to the observed findings and the greater efficiency of combined treatments, a possibility that could be explored in future research.
















