Relationship between hyperglycemia on admission and prognosis in patients with acute myocardial infarction: retrospective cohort study
Acute myocardial infarction (AMI) is one of the diseases with the highest morbidity and mortality in the world. Although timely and effective revascularization and the use of drugs have improved the clinical outcomes of AMI, the mortality rate of AMI remains high. In addition, other clinical factors that affect the mortality of patients with AMI are considered. Hyperglycemia is a universal clinical phenomenon in critically ill patients, and increasing evidence has shown that it is related to disease severity and mortality .
Diabetes promotes the onset and development of AMI. For AMI patients with diabetes, the prognosis is relatively poor and the mortality rate is high. Hyperglycemia on admission is a common phenomenon in patients with AMI. Epidemiological studies have shown that hyperglycemia is present in approximately 25%-50% of patients with AMI and is considered an effective prognostic factor , regardless of whether they have diabetes or not. Subsequent research has suggested that high blood sugar levels on admission could predict a poor short-term prognosis for AMI patients without diabetes and that in-hospital mortality increases with increasing blood glucose levels, but its prognostic value in patients with AMI remains controversial.
To date, no consensus has been reached on the value of hyperglycemia on admission in patients with AMI. The mechanisms of glucose metabolism are different between patients with diabetes and without diabetes, so the cut-off value of serum glucose on admission to predict mortality should be unequal. However, most studies used the same prognostic threshold whether diabetes existed or not, which affected to some extent the predictive effect of serum glucose on admission, especially in patients with AMI and diabetes.
Therefore, this study sought to investigate the significant cut-off value of admission blood glucose for predicting adverse events in AMI patients with or without diabetes, and provide clinicians with a trigger point for glucose-lowering therapy.
Background
The optimal threshold of hyperglycemia on admission to identify high-risk individuals in patients with acute myocardial infarction (AMI) and its impact on clinical prognosis are still unclear.
Methods
We retrospectively reviewed 2027 patients with AMI admitted from June 2001 to December 2012 in the ’Medical Information Mart for Intensive Care III’ database . Significant cut-off values of blood glucose at admission (Glucose_0) for predicting in-hospital mortality in AMI patients with and without diabetes were obtained from the receiver operating characteristic (ROC) curve, then patients were assigned to groups with hyperglycemia and without hyperglycemia according to corresponding cut-off values. The primary endpoints were hospitalization and 1-year mortality.
Results
Among 2027 patients , death occurred in 311 patients (15.3%). According to the ROC curve, the significant cut-off values of Glucose_0 for predicting in-hospital mortality were 224.5 and 139.5 mg/dL in patients with diabetes and without diabetes, respectively.
The crude in-hospital and 1-year mortality of the subgroup with hyperglycemia was higher than that of the corresponding group without hyperglycemia (p< 0.01).
After adjustment, regardless of diabetes status, hyperglycemia on admission was associated with a significant increase in in-hospital mortality in patients with AMI.
For AMI patients without diabetes , hyperglycemia on admission was positively correlated with increased 1-year mortality (HR, 1.47; 95% CI, 1.18 to 1.82; p=0.001). However, this trend disappeared in those with diabetes (HR, 1.35; 95% CI, 0.93 to 1.95; p=0.113).
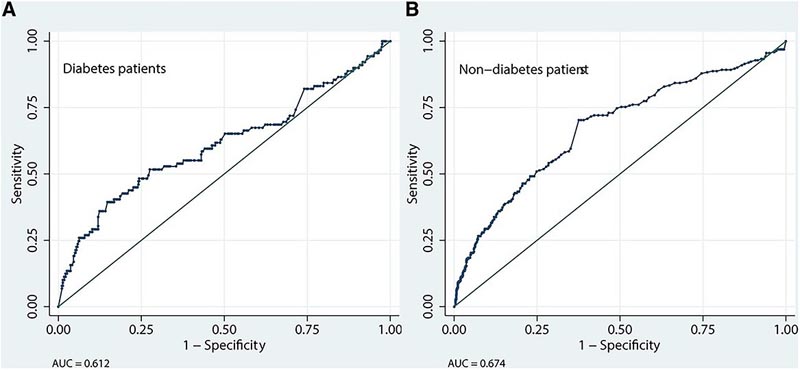
Figure : ROC curve of Glucose_0 predicting in-hospital mortality in patients with AMI. (A) The ROC curve of Glucose_0 for predicting in-hospital mortality of AMI patients with diabetes. (B) The ROC curve of Glucose_0 for predicting in-hospital mortality of AMI patients without diabetes. AMI, acute myocardial infarction; AUC, area under the curve; Glucose_0, blood glucose upon admission; ROC, receiver operating characteristic .
Conclusion
Overall, the predictive value of hyperglycemia on admission was similar between patients with and without diabetes with AMI for in-hospital mortality. However, in terms of long-term prognosis, hyperglycemia on admission was an independent predictor of AMI patients without diabetes , rather than with diabetes.
Therefore, especially for nondiabetic patients with AMI, timely and effective hypoglycemic treatment strategies and nursing measures are very important.
Discussion
This research was designed to analyze the predictive potential of Glucose_0 on prognosis in patients with AMI with and without diabetes, and determine risk stratifications through significant cut-off values. We found that in-hospital mortality in the hyperglycemia group was markedly higher than in the non-hyperglycemia group, whether combined with diabetes or not. In particular, Glucose_0 of ≥139.5 mg/dL was one of the predictors of 1-year mortality in patients with AMI without diabetes. In comparison, hyperglycemia at admission did not predict 1-year mortality in patients with diabetes.
Hyperglycemia on admission is an important and often overlooked condition that can have life-threatening consequences.
Some potential mechanisms may explain the results of our research. Hyperglycemia increases cell adhesion factor, causes leukocyte aggregation in capillaries, shortens the half-life of fibrinogen, increases fibrinogen peptide A and coagulation factor VII, increases platelet aggregation, increases platelet thrombosis, and reduces endothelium-dependent vasodilation, which significantly increases the area of AMI, reducing cardiac function and increasing mortality.
We noted that admission blood glucose and white blood cell count of nonsurvivors were significantly higher than those of survivors. This was consistent with previous studies, indicating that hyperglycemia is related to inflammation . Furthermore, hyperglycemia is also related to an increase in free fatty acids and a prolonged QT interval, leading to the occurrence of ventricular arrhythmia and the elimination of ischemic preconditioning. We observed that the proportion of ventricular arrhythmias in non-survivors was higher, which is consistent with the conclusions of previous research that hyperglycemia was positively correlated with malignant arrhythmias.
What is already known about this topic?
- Hyperglycemia on admission is common in patients with acute myocardial infarction (AMI).
- Hyperglycemia on admission is a predictor of poor short-term prognosis in patients with AMI.
What this study adds
- Hyperglycemia on admission was a marker of high risk of in-hospital mortality in patients with AMI, regardless of the presence or absence of diabetes.
- The significant cut-off value of glycemia on admission to predict in-hospital mortality in diabetic patients with AMI was notably higher than that in non-diabetic patients.
- For 1-year mortality, hyperglycemia on admission was an independent predictor of nondiabetic patients with AMI rather than diabetic patients.
How this study might impact research, practice, or policy
- For nondiabetic AMI patients with hyperglycemia on admission, strict blood glucose control and more aggressive treatment measures should be performed during hospitalization.
Final message Hyperglycemia on admission was an independent predictor of mortality during hospitalization and at one year in patients with AMI, especially in patients without diabetes. |
















